The Impact Of Low- Versus High-Intensity Surveillance Cystoscopy On Surgical Care And Cancer Outcomes In Patients With High-Risk Non-Muscle-Invasive Bladder Cancer (NMIBC)
Michael E. Rezaee, MD, MPH1, Kristine E. Lynch, PhD2, Zhongze Li, MS3, Todd A. MacKenzie, PhD3, John D. Seigne, MBBCh1, Douglas J. Robertson, MD, MPH4, Brenda Sirovich, MD, MS5, Philip P. Goodney, MD, MS4, Florian R. Schroeck, MD, MS4
1Dartmouth-Hitchcock Medical Center, Lebanon, NH, 2University of Utah, Salt Lak City, UT, 3Geisel School of Medicine, Hanover, NH, 4Veterans Affairs Medical Center, White River Junction, VT, 5Veterans Affairs Medical Center, White River Junction, VT
Introduction: Surveillance guidelines for NMIBC are based on expert opinion and informed by limited evidence. We have previously found that about one third of patients with high-risk NMIBC undergo fewer surveillance cystoscopies than recommended (i.e., low-intensity surveillance). Our objective was to assess the association of low- vs. high-intensity cystoscopic surveillance with outcomes, including the frequency of transurethral resections, bladder cancer death, and progression of disease.
Material & Methods: Retrospective national cohort study of patients diagnosed with high-risk (high grade Ta, T1, or carcinoma in situ) NMIBC from 2005 to 2011 within the Department of Veterans Affairs with follow-up through 2014. Patients were categorized by number of surveillance cystoscopies over two years following diagnosis into low- (1-5) vs. high-intensity (6 or more) surveillance. Propensity score adjusted Poisson regression was used to assess the association of low-intensity cystoscopic surveillance with frequency of transurethral resections (overall and resections with or without cancer in the specimen). Propensity score adjusted competing risks regression was used to assess the association of surveillance intensity with risk of bladder cancer death or progression to invasive disease, stratified by whether patients were diagnosed with non-invasive or invasive disease.
Results: Among 1,542 patients, 520 (33.7%) underwent low-intensity cystoscopic surveillance. Those receiving low-intensity surveillance over 2 years following diagnosis underwent a median of 4 cystoscopies, compared to a median of 7 for high-intensity surveillance. Patients undergoing low-intensity surveillance had fewer transurethral resections overall (37 vs. 99 per 100 person years; p<0.001), resections with cancer in the specimen (28 vs. 77 per 100 person years, p<0.001), and resections without cancer in the specimen (7.5 vs. 16 per 100 person years; p<0.001). Low vs. high-intensity surveillance was not associated with risk of bladder cancer death among patients with non-invasive (cumulative incidence 5.8% vs. 8.3% at 5 years, p=0.27) or with invasive disease at diagnosis (cumulative incidence 10.3% vs. 9.6% at 5 years, p=0.75, Figure Panel A). Among patients with non-invasive disease, low-intensity surveillance was unexpectedly associated with a decreased risk of progression or bladder cancer death (cumulative incidence 20% vs. 31% at 5 years, p=0.003, Figure Panel B).
Conclusions: Patients with high-risk NMIBC undergoing low- vs. high-intensity cystoscopic surveillance underwent fewer transurethral resections, but did not experience an increased risk of bladder cancer death. In fact, they had a lower risk of progression. These findings suggest that less intensive surveillance might be reasonable for patients with high-risk NMIBC. However, patients who underwent low-intensity surveillance likely had more favorable bladder cancer, because urologists used clinical information not available in our data to inform their decision making. Thus, these observational data provide a strong rationale for a prospective randomized study to assess whether the frequency of surveillance can be decreased among patients with high-risk NMIBC. 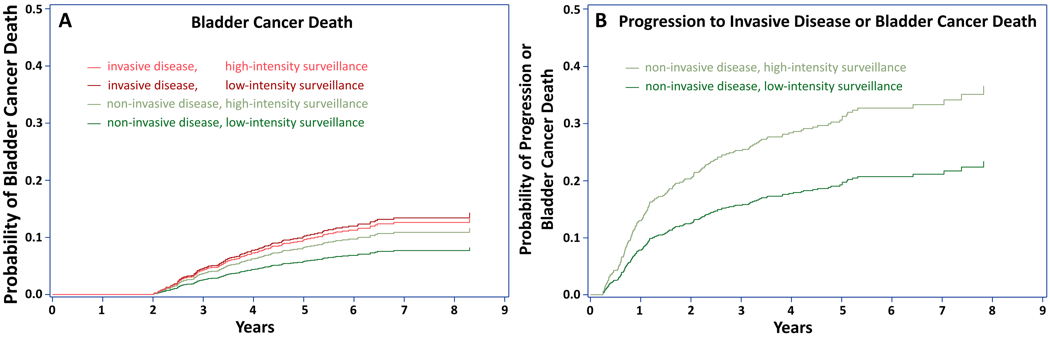
Back to 2019 Abstracts
