The Impact Of Frequent Cystoscopy On Surgical Care And Cancer Outcomes Among Patients With Low-Risk Non-Muscle-Invasive Bladder Cancer
Florian R. Schroeck, MD, MS1, Kristine E. Lynch, PhD2, Zhongze Li, MS3, Todd A. MacKenzie, PhD3, David S. Han, MS1, John D. Seigne, MBBCh4, Douglas J. Robertson, MD, MPH1, Brenda Sirovich, MD, MS1, Philip P. Goodney, MD, MS1
1White River Junction VA Medical Center and and Geisel School of Medicine at Dartmouth, White River Junction, VT, 2VA Salt Lake City Healthcare System and University of Utah, Salt Lake City, UT, 3Department of Biomedical Data Science, Geisel School of Medicine at Dartmouth, Lebanon, NH, 4Section of Urology at DHMC and Geisel School of Medicine at Dartmouth, Lebanon, NH
Background: Surveillance recommendations for patients with low-risk non-muscle-invasive bladder cancer (NMIBC) are based on limited evidence. Our objective was to add to the evidence by assessing outcomes after frequent versus recommended cystoscopic surveillance.
Methods: This is a retrospective cohort study of patients diagnosed with low-risk (low grade Ta) NMIBC from 2005 - 2011 with follow-up through 2014 from the Department of Veterans Affairs. Patients were classified as having undergone frequent versus recommended cystoscopic surveillance (>3 versus 1-3 cystoscopies in the first 2 years after diagnosis). Using propensity score adjusted Poisson regression, we estimated the impact of frequent cystoscopy on the number of transurethral resections and on the number of resections without cancer in the specimen. We used competing risks regression to assess associations between frequent cystoscopy and the risk of progression to muscle-invasive bladder cancer (MIBC) or bladder cancer death.
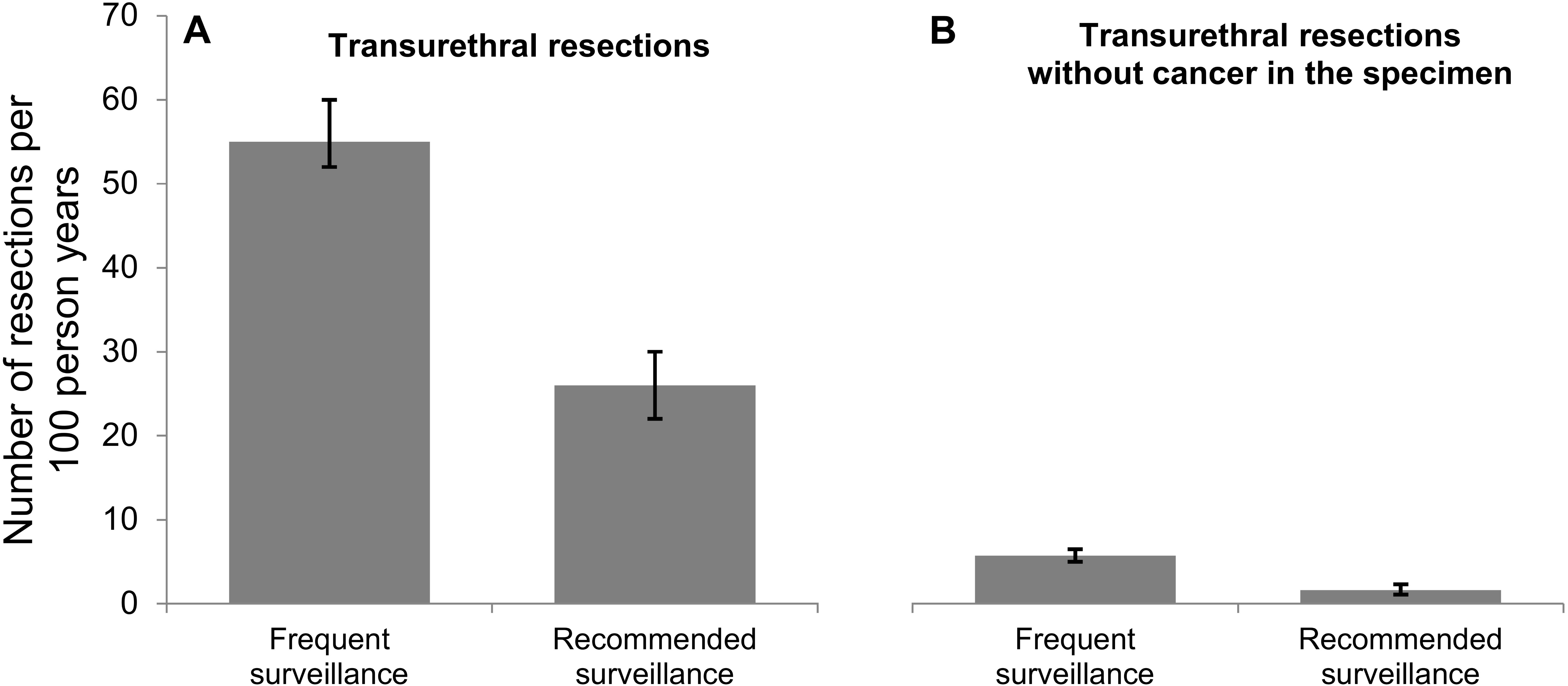
Results: Among 1,042 patients, 798 (77%) had more frequent cystoscopy than recommended. In adjusted analyses, the frequent cystoscopy group had twice as many transurethral resections (55 versus 26 per 100 person years; p<0.001, Figure 1A) and more than 3 times as many resections without cancer in the specimen (5.7 versus 1.6 per 100 person years; p<0.001, Figure 1B). Frequent cystoscopy was not associated with time to progression to MIBC or bladder cancer death (3% at 5.0 years in both groups; p=0.990, Figure 2A) or with time to bladder cancer death (3% at 5.4 years versus 3% at 5.1 years, p=0.817, Figure 2B).
Conclusions: Frequent cystoscopy among patients with low-risk NMIBC was associated with twice as many transurethral resections and did not decrease the risk for bladder cancer progression or death. Frequent cystoscopy may lead to more incidental findings of abnormal appearing areas within the bladder, prompting additional biopsies. Overall, our findings support current guideline recommendations for less frequent cystoscopic surveillance among patients with low-risk NMIBC.

Back to 2019 Abstracts
