Nephrolithiasis is Associated with Depression in US Adults: an NHANES Analysis
Lael Reinstatler, MD, MPH, Vernon Pais, MD; Briana Goddard, BA
Dartmouth Hitchcock Medical Center, Lebanon, NH
Background: Depression and anxiety have been associated with increased number of opioid prescription refills among those managed with opioids for myriad problems including nephrolithiasis. Furthermore, depression and anxiety are independent risk factors for opioid abuse. Given frequent use of opioids in treating nephrolithiasis, we sought to determine the prevalence of anxiety and depression among stone formers.
Methods: We conducted a population-based survey analysis of the National Health and Nutrition Examination Surveys (NHANES) from 2013-2016. We included all adults and examined sociodemographic factors including responses to survey questions regarding history of nephrolithiasis, anxiety, depression, and overall health status.
Results: In an analysis representing nearly 117,000,000 US adults, there was a 9.1% prevalence of nephrolithiasis. While 20% of the population denied any anxiety symptoms, 47% reported occasional symptoms, 18% reported weekly, and 16% reported daily anxiety. Half of the population denied depression symptoms while 40% reported occasional symptoms, 6.5% reported weekly, and 4.3% reported daily. Nine percent of the population seeks regular mental health care. Among the total population, 14% report excellent health, 60% report very good/good, and 18% report fair/poor. When stratified on a history of nephrolithiasis vs none, there were higher rates of anxiety and depression symptoms, but these were not significant (83% vs 80.5% p = 0.3370, 58.5% vs 52.3%, p = 0.0690). However, those with nephrolithiasis had significantly higher rates of treatment by mental health providers (11.6% vs 8.7%, p = 0.0324) and reported worse health status (26% fair/poor vs 18%, p<0.0001). On logistic regression controlling for age, race, BMI, and gender, patients with nephrolithiasis had higher rates of depression with an OR of 3.2 (1.03, 9.77) for daily, 2.06 (1.13, 3.75) for weekly, and 1.32 (0.96, 1.82) occasionally compared to never (p = 0.0463 overall). Patients with nephrolithiasis also reported overall lower health scores (p<0.0001).
Conclusion: A diagnosis of nephrolithiasis is associated with higher rates of depression, mental health care, and perceptions of lower reported health status. Providers should be vigilant for signs and symptoms of depression and anxiety in those they see for kidney stones. In light of the increased risk of comorbidities including opioid abuse, mental health referral should be pursued for those stone formers reporting symptoms of depression and anxiety. 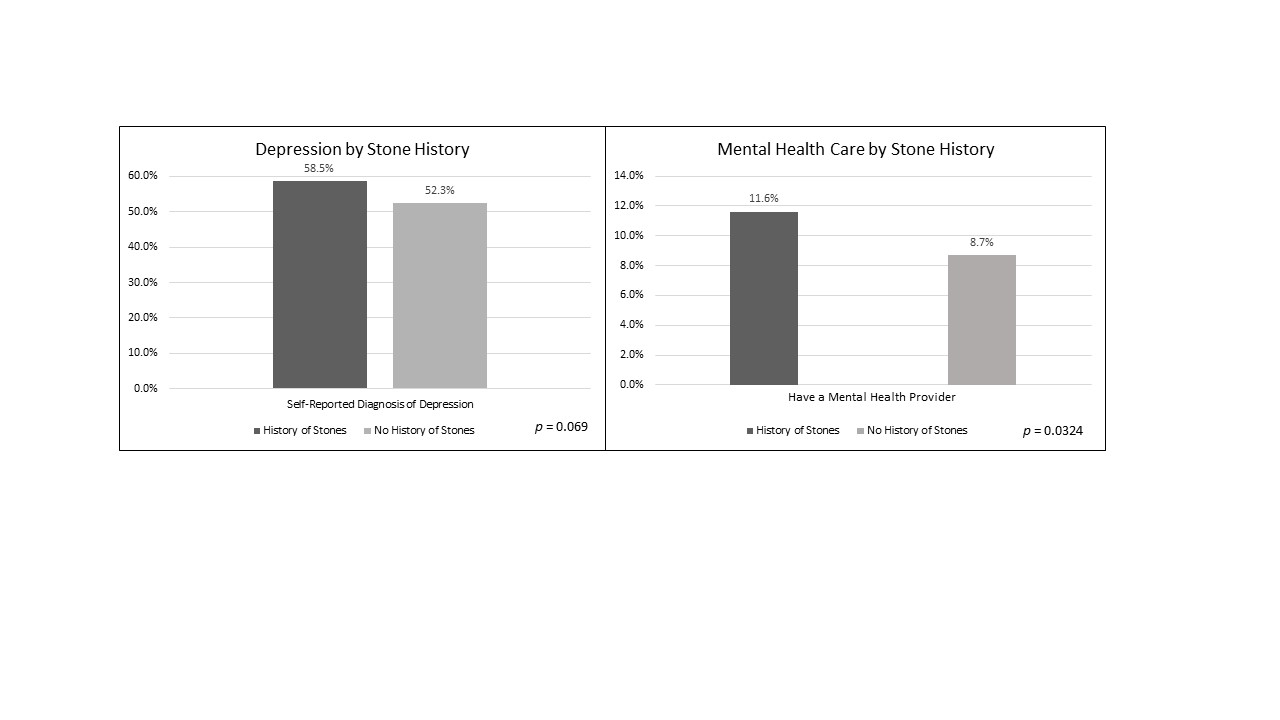
Back to 2019 Abstracts
