Creation and initial implementation of the D.I.R.E.C.T Pathway (Delayed Imaging to Reduce Excessive Computed Tomography) for the evaluation of patients with suspected renal colic
Kevan M. Sternberg, MD, David W. Sobel, MD, Aaron Greenspun, BS, Roz Bidad, BSN, Peter Weimersheimer, MD
University of Vermont, Burlington, VT
BACKGROUND: Computed tomography (CT) remains the standard of care for the evaluation of acute renal colic and its use has significantly increased over the past 2 decades. Concerns, however, exist regarding radiation exposure and cost. Ultrasonography has been proposed as an alternative initial imaging approach. While shown to be safe, urologists often require the additional anatomic information provided by CT to help guide patient management. Considering that the majority of ureteral stones (~80%) will pass without intervention, obtaining a CT initially on every patient with a suspected stone may not be necessary. We propose an ED algorithm using initial ultrasonography for patients with high suspicion of uncomplicated ureterolithiasis that provides a mechanism for appropriate outpatient urologic follow-up with CT imaging if necessary. Methods: A prospective study was approved by the UVM IRB and an algorithm was developed defining patient eligibility, screening, diagnostic evaluation, discharge instructions, and follow-up supported through an internal grant at the University of Vermont (Figure 1). Through funding, a research coordinator was hired to organize workflow, collect data, and contact patients to arrange follow-up after the ED visit. Patient eligibility is determined by the STONE score and/or clinical judgement of the likelihood of the presenting symptoms being secondary to a stone. For those with a high suspicion, an ultrasound is obtained. If the presenting symptoms are controlled with no change in suspected diagnosis, the patient is discharged home with specific instructions and a urinary strainer. Follow-up phone calls occur at day 1-2 and day 7-10 post discharge. If there is no definitive stone passage and/or persistent symptoms, an outpatient urology visit is initiated that includes a reduced dose CT prior. Results: The pathway began January 2019. To date, 5279 patients have been screened, 436 have met initial inclusion criteria, and 20 have been enrolled. The average STONE score of those enrolled was 9.6. Ten (50%) had a STONE score < 10. Thus far, 2 patients passed a stone after initial US and avoided CT. 6 patients had a CT after US, 3 while still in the ED. 10 patients had US alone (2 passed a stone, 1 to OR , 7 unable to be reached). Of the patients who could not be reached, review of the electronic health record did not reveal any ED return visits or CTs obtained. 3 patients are awaiting follow-up. Conclusion: Our initial results show that through a coordinated effort between Urology and Emergency Medicine, our pathway is feasible to implement and initial results are promising regarding the reduction of upfront CT scans obtained. Patient follow up/compliance is one concern. The utility of the STONE score is another question as the majority of patients enrolled did not meet the criteria for likely ureterolithiasis. Future results are needed to evaluate the success of our pathway and determine whether this model can be expanded outside of our single center experience. 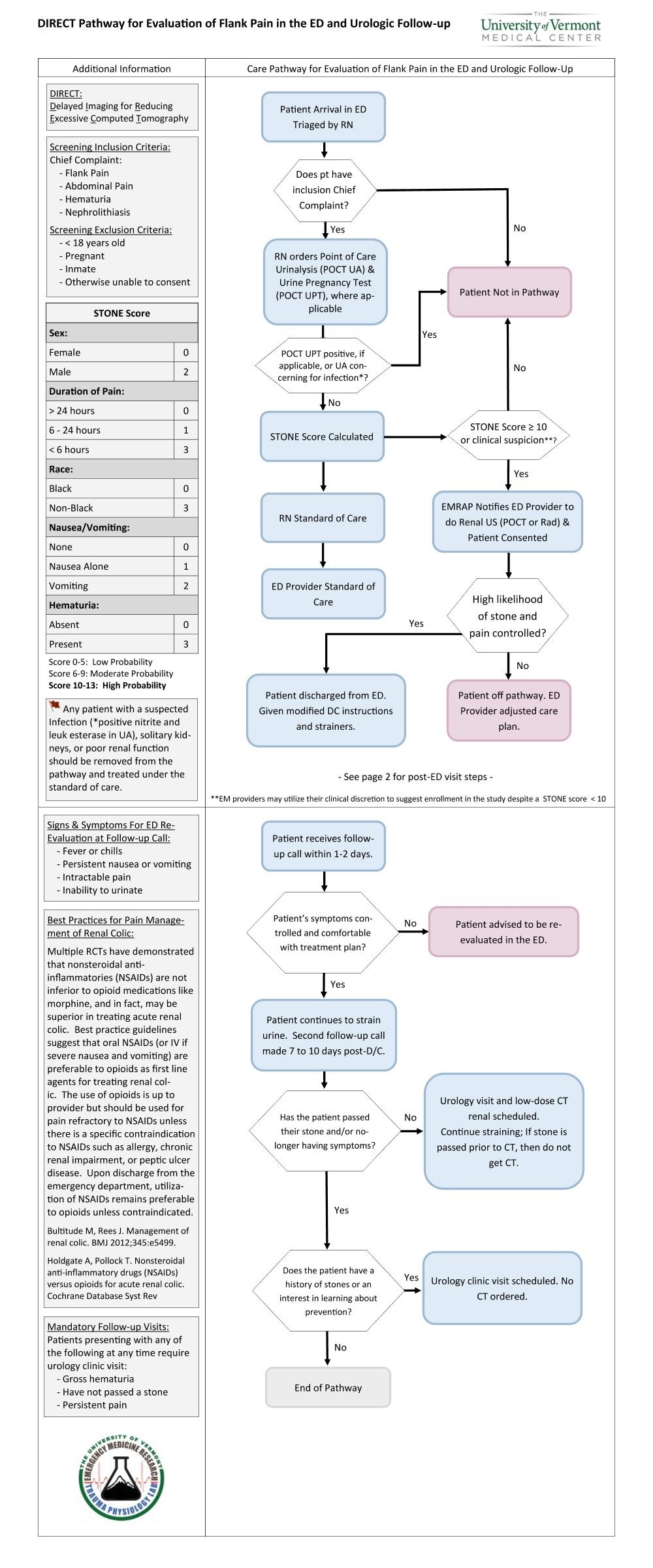
Back to 2019 Abstracts
