Impact of a Multidisciplinary Kidney Stone Prevention Clinic
Kevin Krughoff, MD1, Cassandra Delude, APRN2, Kathy Burzynski, RD2, Scott Fabozzi, MD3
1Dartmouth-Hitchcock, Lebanon, NH, 2Concord Hospital, Concord, NH, 3Concord Hospital, Lebanon, NH
Introduction: There are several known benefits of a multidisciplinary approach to stone prevention, however the implementation of this model in the community setting has not been described. Our goal was to assess the feasibility of a stone prevention clinic in a community-based practice using responses to questionnaires, 24-hour urine parameters and routine imaging results.
Materials and Methods:
Patients with recurrent stone disease, risk factors or comorbidities that place restrictions on their diet were enrolled in the stone prevention clinic. Appointments included a review of patient history, medications, dietary habits, stone analysis, lab work and 24-hour urine results. Patients were met with an APRN and Registered Dietitian (RD) who used this information to create personalized dietary and lifestyle plans. Patients were administered a questionnaire to determine how beneficial they felt the clinic was. Questionnaire results, stone risk parameters and imaging results were retrospectively reviewed for all consecutive patients referred to the clinic. Paired-samples t-tests were used to assess changes in individual 24-hour urine parameters across follow up visits. For patients with prior 24-hour urine data, difference-in-difference testing was used to assess change in stone supersaturation trends following enrollment.
Results:
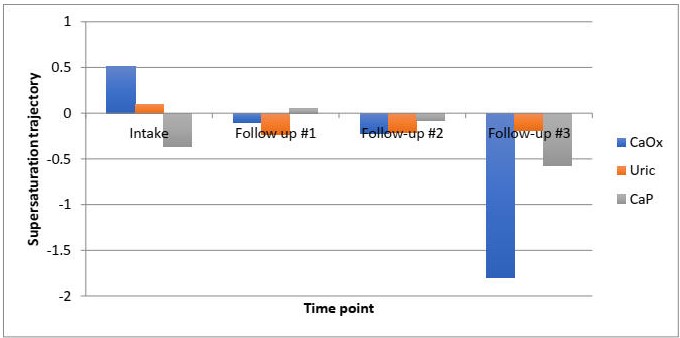
77 patients were followed over an average of 1.76 follow up visits (275±143 days). Of the 63 surveys completed, 100% of patients found their visit with the RD helpful and 98.4% would recommend the clinic to friends/family. Of the 46 records with consecutive 24-hour urine studies, significant reductions were observed in the supersaturation profiles for uric acid (-0.301±0.089, p<0.01) and calcium phosphate (-0.6416±0.298 p=0.04) (Table 1). A significant decrease was seen in the trajectory of uric acid supersaturation following enrollment (-.371±0.158, p=0.02) (Figure 1). Follow up KUB and renal US showed no stone growth in 95% of patients.
Conclusion:
The implementation of a multidisciplinary stone prevention model is feasible in the community setting. This is supported by positive feedback, significant reduction in stone risk parameters and lack of stone growth on routine imaging.
Table 1. Change in stone supersaturation and supersaturation trajectory.
| Stone Risk [Ref. Range] | Change in Value | 95% CI | Change in Trajectory | 95% CI |
| Calcium Oxalate [6-10] | -0.343 (p=0.57) | -1.49 to 1.45 | -1.271 (p=0.24) | -3.47 to 0.93 |
| Uric Acid [0-1] | -0.301 (p=0.001) | -0.119 to -0.482 | -0.371 (p=0.027) | -0.045 to -0.697 |
| Calcium Phosphate [0.5-2] | -0.642 (p=0.042) | -0.025 to -1.258 | 0.139 (p=0.79) | -0.951 to 1.229 |
Back to 2019 Abstracts
