The Utility and Value of Immersive Virtual Reality Simulation for Percutaneous Nephrostomy Tract Access and Surgical Training
Sehar Resad, MS, Egor Parkhomenko, MD, David S. Wang, MD, Shaun E. Wason, MD.
Boston University School of Medicine, Boston, MA
Background: Percutaneous nephrolithotomy (PCNL) is the gold standard for the removal of large kidney stones. Gaining renal access into the desired calyx is critical for successful stone clearance and is a difficult technique to master. Current methods to train urologists in PCNL access are limited and include bench models, animal kidneys, live porcine models, and simulators. Immersive virtual reality (VR) technology with haptic feedback offers a potentially better training model for surgical learning and proficiency. We sought to evaluate the efficacy of a novel immersive VR simulator for PCNL tract access.
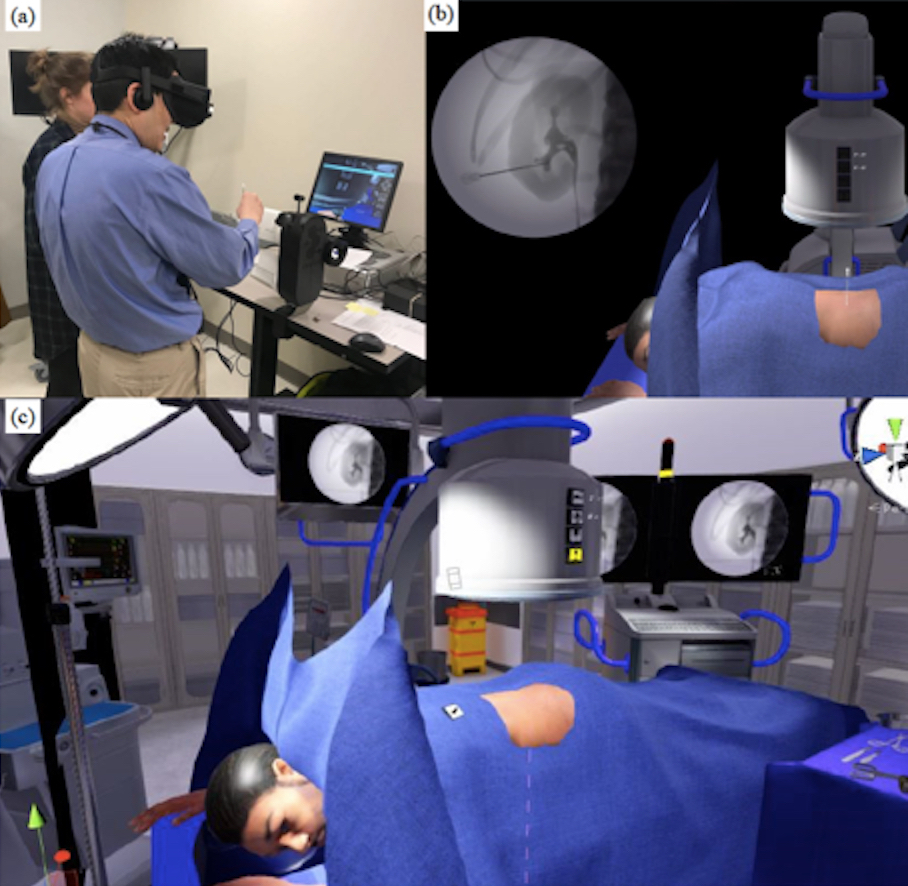
Methods: Urology and interventional radiology (IR) residents and attendings were recruited to evaluate an immersive VR simulator for percutaneous tract access acquisition (Table 1). Using a head mounted display (Oculus Rift) and a robotic arm (Marion Surgical), participants were instructed to establish percutaneous access into the lower pole calyx in the prone position in a VR operating room (Figure 1). A Likert type scale (1 = not at all, 5 = extremely, and 1 = poor, 5 = excellent) was used to record the participant’s VR experience. Additionally, the robotic arm recorded kinematics parameters (economy of motion; cumulative time, path length, and velocity).
Results: Almost all (95%) of the participants rated the VR simulation as a realistic experience. The realism of instrument handling (2.7/5), targeting (3.4/5), haptic feedback (2.4/5) and overall realism (3.25/5) were rated as slightly to somewhat realistic (Table 1). The image quality (4.1/5), brightness (4.3/5), resolution (3.95/5), delay (4.05/5), overall comfort (3.9/5) and overall performance (3.95/5) were rated as very good. The usefulness of the simulator for hand-eye coordination (3.8/5), usefulness as a rehearsal tool (3.8/5), and likelihood to recommend it to colleagues for training (3.6/5) were rated as very good. There were no significant differences between the novices and experts for their VR experience nor economy of motion (cumulative time, path length, and velocity). Subjectively, participant’s comments included that the VR simulator was a great practice module, was realistic and great for ‘warm up’ prior to surgery.
Conclusions: Immersive VR simulation for PCNL access is a unique platform for surgical education which was rated favorably amongst participants. The training platform was unable to differentiate between novices and experts. Further technical improvements to haptic feedback, fluoroscopic control and subsequent procedural steps are warranted. It is likely that future iterations of this technology will help train urologists in PCNL access.
Table 1: Demographics, Virtual reality experience, image control, and economy of motion of an immersive virtual reality simulator for percutaneous nephrostomy tract access
| Demographics (n = 20) | ||||
| Age (year) | 35 (26 - 66) | |||
| Gender (male) | 65% | |||
| Participants Attendings Residents | 6 (IR = 2, Urology = 4) 14 | |||
| Virtual Reality Experience (1 = not at all, 5 = extremely) | ||||
| Total (n=20) | Novice (n = 17) | Expert (n = 3) | p | |
| Realistic (yes) | 95% | 94.1% | 100% | |
| Realism of instrument handling vs live surgery | 2.7 | 2.6 | 3.3 | 0.57 |
| Realism of targets (i.e. calyx, collecting system, etc.) | 3.4 | 3.2 | 4.3 | 0.24 |
| Realism of haptic feedback | 2.4 | 2.2 | 3.3 | 0.20 |
| Overall realism | 3.25 | 3.3 3.7 | 3.0 | 0.77 |
| Usefulness for hand-eye coordination | 3.8 | 4.3 | 0.49 | |
| Useful rehearsal tool | 3.8 | 3.6 | 4.3 | 0.44 |
| Likelihood to recommend | 3.6 | 3.5 | 4.3 | 0.40 |
| Image Control (1 = poor, 5 = excellent) | ||||
| Total (n=20) | Novice (n = 17) | Expert (n = 3) | p | |
| Quality | 4.1 | 4.1 | 4.3 | 0.51 |
| Brightness | 4.3 | 4.3 | 4.3 | 0.94 |
| Resolution | 3.95 | 3.9 | 4.3 | 0.46 |
| Delay in image display (5 = no delay) | 4.05 | 4.1 | 4.0 | 0.92 |
| Overall comfort | 3.9 | 3.9 | 4.0 | 0.87 |
| Overall performance | 3.95 | 3.9 | 4.3 | 0.46 |
| Economy of Motion | ||||
| Total (n=20) | Novice (n = 17) | Expert (n = 3) | p | |
| Cumulative time (s) | 180 | 174 | 214 | 0.55 |
| Path length (cm) | 273 | 275 | 261 | 0.87 |
| Average velocity (cm/s) | .0019 | .020 | 0.015 | 0.36 |
Figure 1: Virtual Surgery Simulator (a) VR simulator set up and use (b) fluoroscopic image with target access (c) virtual operating room seen by participant
Back to 2019 Abstracts
