Cutting the Cord: A National Survey on Urology Resident Vasectomy Training
Mary E. Soyster, BA, Kathryn Wagner, MD, Christian Bartels, MD, Brooke A. Harnisch, MD
University of Connecticut, Farmington, CT
BACKGROUND: Vasectomy is one of the most common in office procedures performed by urologists. Vasectomy is generally performed under local anesthesia while the patient is awake in a urology clinic. This makes the procedure technically challenging and difficult to teach to urology residents. There has been limited research on resident training in vasectomy. Nguyen et. al(1) demonstrated that supervised resident performance of in office vasectomy was safe and well tolerated by patients. To date, no other study on vasectomy training of urology residents exist. The aim of this study was to understand the current vasectomy training environment, including potential barriers to teaching this procedure.
METHODS: An anonymous 18-question survey was e-mailed to the program coordinators of 135 ACGME accredited urology residencies in the United States. The survey was sent via SurveyMonkeyTM and inquired about quantity, comfort and environment of vasectomy training in these programs as well as demographic data.
RESULTS: Overall there were 115 residents respondents. Every AUA section and post-graduate year were represented. 65% of residents had performed ten or more vasectomies by the time they graduated from residency. Despite this, 69.7% of first year urology residents (Uro 1ís), 37% of Uro 2ís, 10.7% of Uro 3ís and 10.7% of Uro 4ís had performed <10 vasectomies. Additionally, 24.4% reported no training in pre and post op vasectomy counseling. A majority of the residents conducted vasectomies in the office versus the operating room. Despite this finding, a statistically significant percentage of resident respondents felt more comfortable performing vasectomies in the OR than in the office setting (89.6% vs 66%, p=<.001.) Common barriers identified to vasectomy training are seen in Table 1. Overall, 76% of residents felt there was enough opportunity to perform vasectomies at their training program despite no formal vasectomy training program or simulation lab.
CONCLUSIONS: Despite the difficulty of teaching vasectomy in an office setting, a majority of residents feel comfortable doing an office vasectomy on their own. However, most urology residency programs have no formal training and residents are less comfortable performing vasectomies in the office when compared to the OR. Additionally, many residents receive no training on counseling. Barriers to training included volume, accessibility of the procedure and autonomy- all highlighting areas for improvement at these institutions. Formal training programs in peri-operative counseling, vasectomy procedure and simulation lab could improve resident comfort and break down barriers to resident training.
1) Nguyen CT, Hernandez AV, Gao T, Thomas AA, Jones JS. Office Based Vasectomy Can be Performed by Supervised Urological Residents With Patient Pain and Morbidity Comparable to Those of a Staff Surgeon Procedure. Journal of Urology. 2008;180(4):1451-1454. Doi:10.1016/j.juro.2008.06.047. 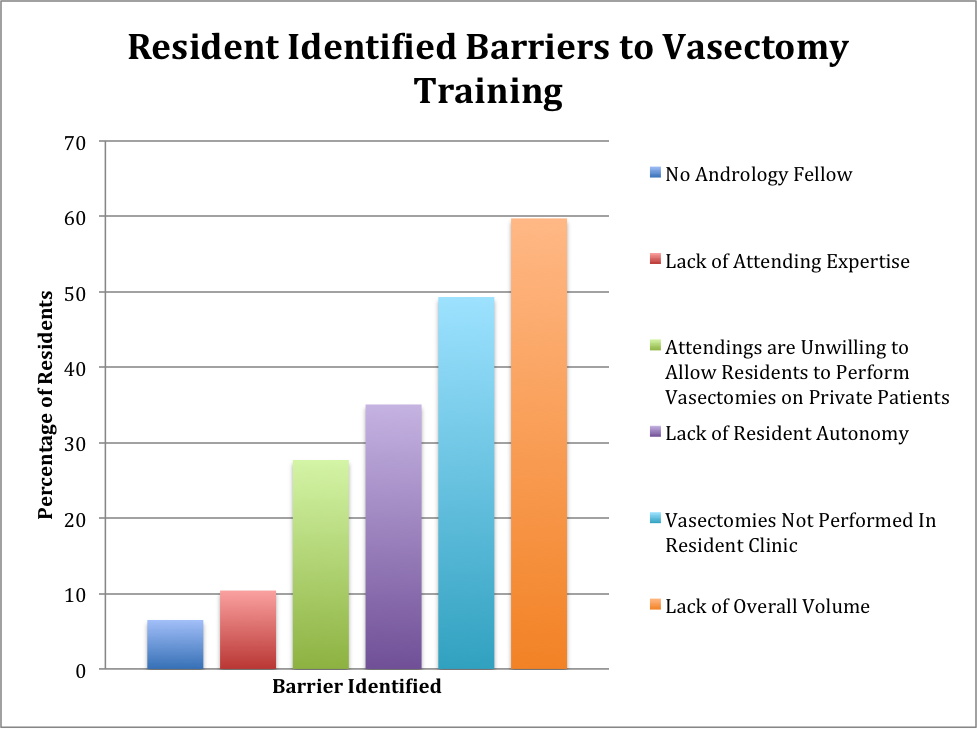
Back to 2019 Abstracts
