Combination of Multiparametric MRI-Ultrasound Fusion and Systematic Prostate Biopsy Results in Optimal Concordance with Final Surgical Pathology
Alice Yu, MD, Tammer Yamany, MD, Nawar Hanna, MD, Eduoard Nicaise, BS, Amirkasra Mojtahed, MD, Mukesh Harisinghani, MD, Chin-Lee Wu, MD, Douglas Dahl, MD, Matthew Wszolek, MD, Michael Blute, MD, Adam Feldman, MD
Massachusetts General Hospital, Brigham and Women's Hospital, Boston, MA
Introduction and Objective: Accurately predicting the Gleason score (GS) on radical prostatectomy (RP) with prostate biopsy is important for risk stratification and selecting patients for active surveillance. Multiparametric MRI (mpMRI) is useful for detecting clinically significant disease, but the exact concordance of GS between fusion biopsy and RP has not been well described in a clinical practice setting. The objective of this study is to assess whether systematic, targeted or combination (targeted + systematic) biopsy has better concordance with final surgical pathology.
Methods: In our institutional mpMRI-ultrasound fusion biopsy database of 570 men, 174 men who underwent targeted and systematic biopsy followed by RP. GS on targeted, systematic and combination (targeted and systematic) biopsy were compared with GS on RP, and concordance was recorded. Concordance rates between biopsy types were compared with the McNemar test. Proportion of GS upgrade or downgrade at time of RP was also evaluated.
Results: Concordance, upgrade, and downgrade rates are reported in Figure 1. Combination biopsy was superior to both systematic [Risk Ratio (RR) 1.25, 95% confidence interval (CI) 1.08 - 1.44, P=0.003] and targeted biopsy (RR 1.22, 95% CI 1.08 - 1.37, P=0.002) for predicting concordance with surgical pathology. There was no significant difference in concordance rates between systematic and targeted biopsy alone (P=0.90). The relative risk of upgrade on surgical pathology with combination biopsy was significantly lower when compared to systematic (RR 0.58, 95% CI 0.48-0.70, P<0.001) or targeted biopsy alone (RR 0.67, 95% CI 0.57-0.79, P<0.001).
Conclusions: Combination (targeted and systematic) biopsy is associated with the highest concordance rate between biopsy and RP when compared with systematic or targeted biopsy alone. When the pathology is non-concordant, standard and targeted-alone biopsy are more likely to underestimate final RP pathology. These data support using a combination of targeted and systematic biopsy as standard practice when doing fusion biopsy. 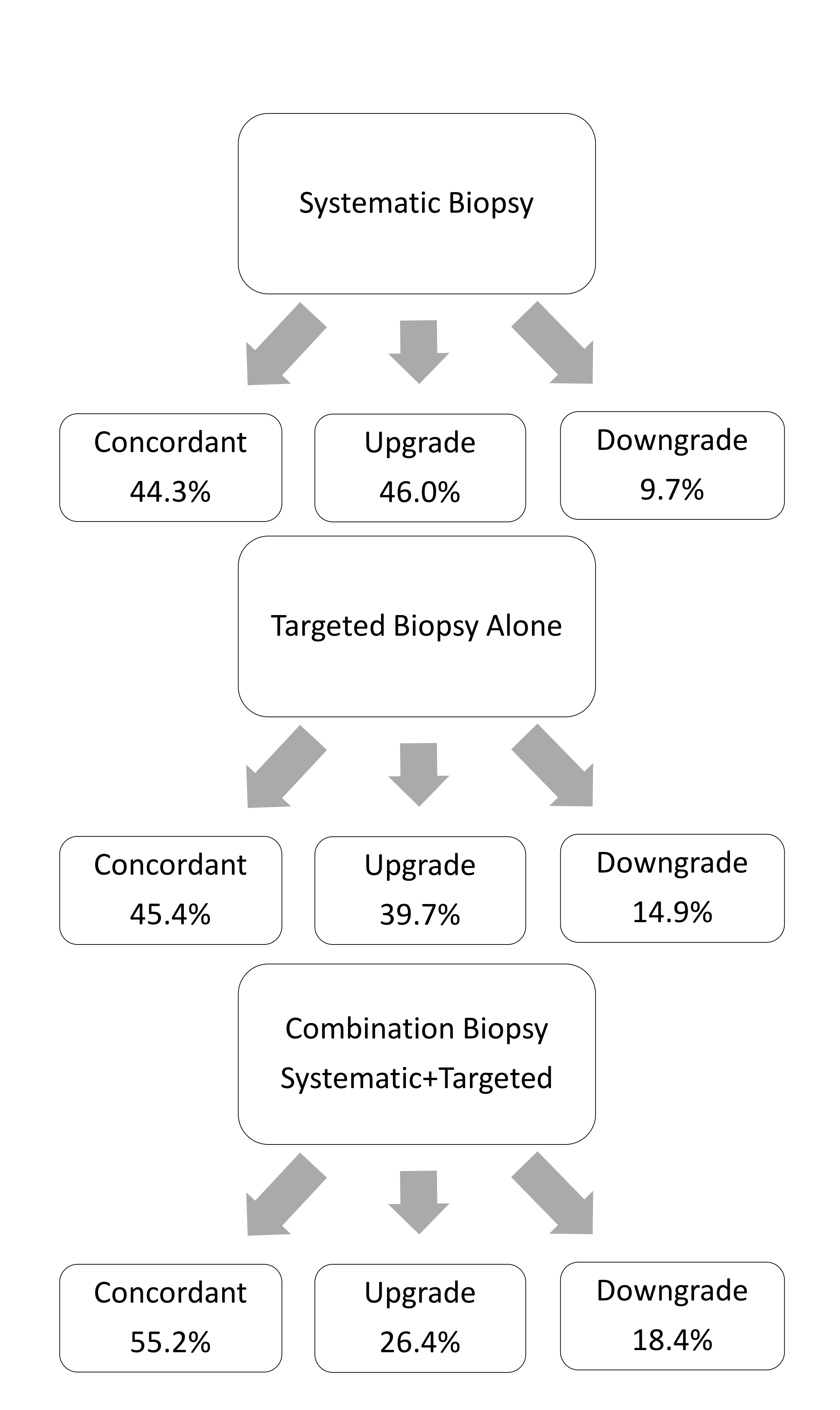
Back to 2019 Abstracts
