Initial Experience of MRI-Fusion Biopsy in the Community Setting
Kevin Krughoff, MD1, Lawrence Dagrosa, MD1, Amichai Kilchevsky, MD2
1Dartmouth-Hitchcock, Lebanon, NH, 2Concord Hospital, Lebanon, NH
BACKGROUND:
The expanding role of MRI-fusion biopsy (FB) is well documented, however the reproducibility of outcomes during the initial experience of FB in the non-academic (NA) is unknown. We sought to determine if there are differences in the yield of clinically significant cancer on FB at an academic versus a NA setting.
METHODS:
We compared fusion-directed and template-directed biopsy cores for the first consecutive 125 FB patients at an academic to the first 125 consecutive FB patients at a NA setting. All patients underwent multiparametric MRI and were scored using PIRADS v.2. Specimens were graded according to the International Society of Urological Pathology (ISUP) criteria for Grade Group (GG). Clinically significant prostate cancer (csPCa) was defined as GG≥2. Patients at the NA setting were matched to academic setting controls using Mahalonobis-distance kernel matching. The following covariates were used: Prior negative biopsy, active surveillance, PSA density, abnormal DRE, family history of prostate cancer, age, use of a 5-alpha reductase inhibitor, BMI, and composite AUA-SS. Patients with pre-existing csPCa or prior treatment were excluded from analysis. Standard errors and the 95% CI were calculated from 3,000 bootstrap samples to determine the effect of NA setting on FB outcomes. Secondary analysis of imaging and pathology characteristics was performed using weighted samples t-tests for continuous variables and pearson chi-square for discrete variables
RESULTS:
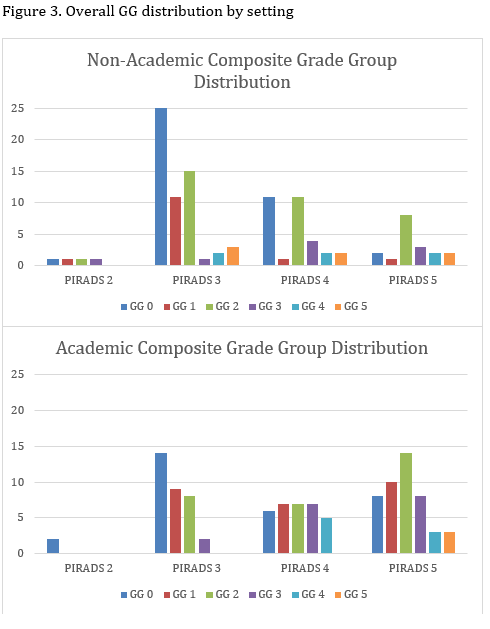
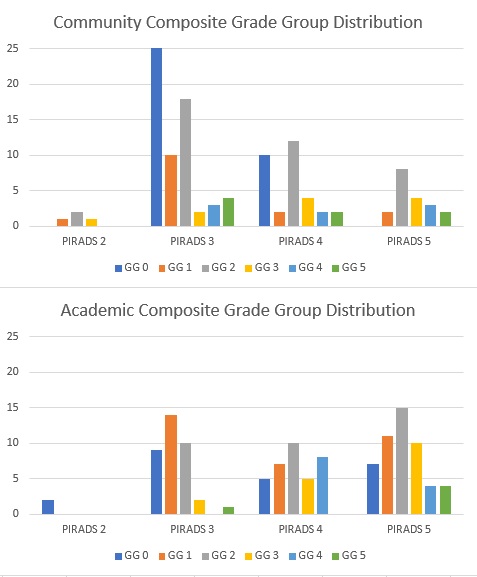
Of the 250 patients included, 219 patients were matched. There were significant baseline differences in frequency of prior negative biopsy and BMI. Matching reduced the difference in means for all covariates. Balance was confirmed by reduction in standardized differences and variance ratios (Fig.1). There was no significant effect of NA setting on the proportion of FB-detected csPCa, the proportion of template-detected csPCa, the rate of upgrading from prior biopsy results, or in the proportion of csPCa missed by fusion-directed or template-directed cores (Table 1). On average, lesions were given lower PIRADS ratings in the NA setting and template biopsies yielded lower GG diagnoses, however the maximum composite GG was not significantly different by practice setting (Figures 2, 3).
CONCLUSIONS:There was no significant effect of practice setting on the detection of clinically significant cancer in a sample-matched analysis of the first consecutive patients to undergo fusion biopsy. 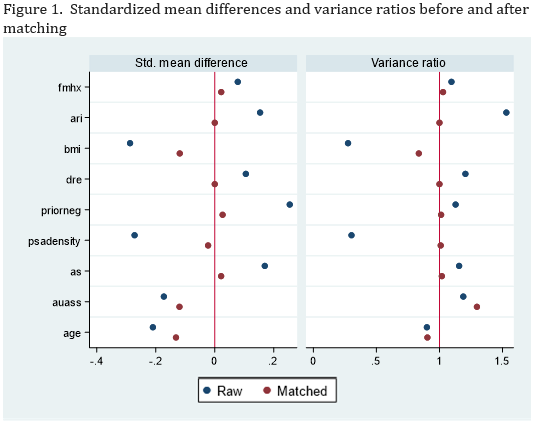

Back to 2019 Abstracts
