Associations of Rurality and Disease Outcome in Urologic Malignancy
Marianne Casilla-Lennon, MD, Alejandro Abello, MD, Patrick A. Kenney, MD, Michael Leapman, MD
Yale School of Medicine, New Haven, CT
ASSOCIATIONS OF RURALITY AND DISEASE OUTCOME IN UROLOGIC MALIGNANCY
INTRODUCTION
Patients residing in rural regions have comparatively worse outcomes for many cancers. However there is less known about treatment and outcome for patients with urologic cancers. The objective of this study is to evaluate differences in treatments and outcomes among patients with urologic malignancies when coming from rural compared to metropolitan communities using national, population-level data.
METHODS
We queried the Surveillance, Epidemiology and End-Results database to identify patients with urological cancers from 1973 to 2015. We compiled patient clinical, demographic, and outcome data, including rurality at the county level. Rural counties is defined as those with >50% population living in rural areas. We evaluated the association of rurality with treatment received, presence of advanced disease, and cancer-specific death using descriptive statistics and Cox proportional hazard models.
RESULTS
We identified 992,536 patients including those with Kidney (112,477), Bladder (208,230), Prostate (637,005), penile (6,297) and testis cancer (28,527). Among all patients, 898,050 (90.4%) were male and 64,992 (6.55%) lived in rural counties. Overall, patients living in rural communities were older at cancer diagnosis (mean 70 ± 12.1 vs 67.41 ± 12.7) and more frequently of white race (97.1% vs 82.46%) vs urban counterpart. Patients residing in rural counties were less likely to undergo definitive treatment with surgery for stage 1 or stage 2 disease (p <0.001). In multivariable Cox regression, rural status was associated with greater risk of cancer-specific death in kidney cancer (HR: 1.1, 95% CI: 1.02-1.24; P value: 0.03) but was not seen in other cancers (Figure 1). After categorizing the population based on % of rurality, adjusted kidney cancer-specific death increased among most rural populations: 15% rurality or more (HR: 1.16, 95% CI: 1.05-1.27; P: 0.03), 40% rurality or more (HR: 1.31, 95% CI: 1.15-1.49; P < 0.001) and 70% or more (HR: 1.32, 95% CI: 1.05-1.67; P value: 0.01)
CONCLUSION
There are notable differences in cancer incidence, treatment and outcome for patients residing in rural areas. Rural status was associated with poorer cancer-specific survival for kidney cancer but was not seen in other genitourinary malignancies, independent of stage at diagnosis and treatment received. Further research is warranted to understand the factors underlying these differences in outcome.
Figure 1 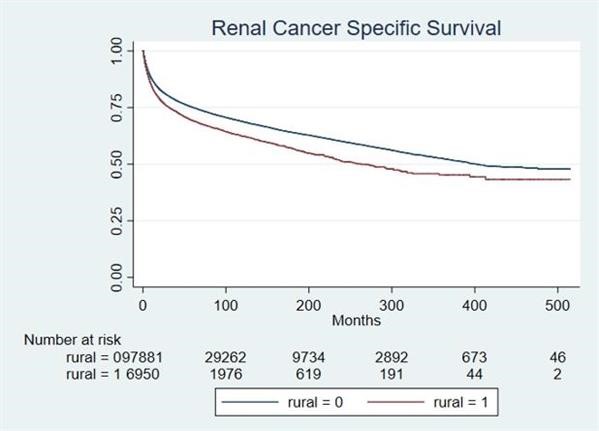
Back to 2019 Abstracts
