Impact Of Second Generation Neoadjuvant Hormone Therapy On Radical Prostatectomy Outcomes
Alice Yu, MD1, Julie Szymaniak, MD1, Melissa Huynh, MD1, Dimitar Zlatev, MD1, Rana McKay, MD2, Mary-Ellen Taplin, MD3, Adam Kibel, MD1
1Brigham and Women's Hospital, Boston, MA, 2University of San Diego, San Diego, CA, 3Dana Farber Cancer Institute, Boston, MA
Introduction and Objective: Phase II trials have shown that intense neoadjuvant androgen deprivation therapy (NeoADT) with abiraterone or enzalutamide combined with luteinizing hormone-releasing hormone (LHRH) analogues demonstrate favourable pathologic response in prostate cancer. There are currently phase III trials underway. However, the impact on surgical complication rates as well as the impact of therapeutic response on complication rates is unknown. The objective of this study is to assess complication rates and functional outcomes in patients who received NeoADT followed by radical prostatectomy (RP).
Methods: Between November 2014 and August 2018, 90 men with intermediate or high-risk prostate cancer were enrolled in two clinical trials involving 6 months of intense NeoADT followed by RP (figure 1). Data on surgical complications, pathology and self-reported functional outcomes were collected. Self-administered SHIM and EPIC questionnaires were used to assess post-operative erectile function. Comparison between nerve-sparing (NS) groups were performed using Fisher’s exact tests.
Results: Mean surgery time was 173 ± 42.2 minutes. Post-operative length of stay was 1 day in 87.8% of cases. Thirteen men (14.4%) experienced a post-operative complication; all except one were minor (≤ Clavien Grade II). We were able to perform bilateral or unilateral NS procedure in 24 (27%) and 36 (41%) cases respectively. NS did not result in higher positive margin rates (NS vs. non-NS, 13.3% vs 13.8%, P=1.0) possibly related to patient selection.
Prior to surgery, 38% of men reported potency, 5% used assistance and 20% had erectile dysfunction. Pre-operative potency status was unknown for 37% of our cohort. At median time of 1-year post-RP, 24% of those who underwent unilateral or bilateral NS surgery regain mild to moderate erectile function on self-reported questionnaires, compared to 0% in those who did not receive NS surgery.
As for urinary incontinence, 62.7% (52/83) of men reported using zero pads per day at 6 months, and this increased to 71.9% (46/64) at 1 year. Additionally, 81% and 97% reported using 1 pad per day or less at 6 months and 1 year respectively. This was not significantly different between NS groups (P=0.57).
Among ypT0 patients, 82% received NS surgery. 70% reported mild to moderate potency at 1-year post-RP compared to 12% of those with higher residual disease (P<0.001). ypT0 patients had similar continence rates as patients with higher residual disease with only 1 patient using more than 1 pad per day in each group.
Conclusions: Post-operative complication rates were low, even after aggressive NeoADT. Patients with complete pathologic response to NeoADT were more likely to receive NS surgery.
Word count: 442/500 (25 for image)
Figure 1 - Neoadjuvant Androgen Deprivation Therapy Protocol 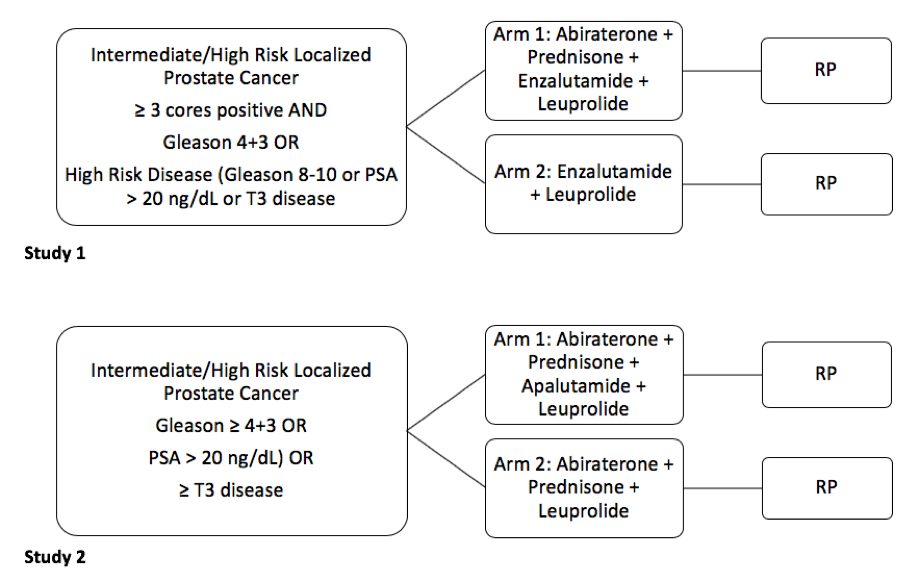
Back to 2019 Abstracts
