Widespread Use Of Multiparametric MRI In An Active Surveillance Cohort Results In Earlier Identification And Treatment Of Clinically Significant Prostate Cancer
Alice Yu, MD, Andrew Gusev, BS, Timothy Baloda, BS, Eduoard Nicaise, BS, Mukesh Harisinghani, MD, Amirkasra Mojtahed, MD, Douglas Dahl, MD, Matthew Wszolek, MD, Anthony Zietman, MD, Adam Feldman, MD, MPH
Massachusetts General Hospital, Boston, MA
Introduction: Multiparametric MRI (mpMRI) has led to improved detection of clinically significant prostate cancer and is now increasingly used in active surveillance (AS) patients. However, most AS cohorts in the literature were described prior to widespread use of mpMRI. Our investigation compares outcomes in AS in the pre- and post-MRI era at our institution.
Methods: We used an institutional database of 1291 men who started AS between September 1996 to December 2016. The cohort was divided into pre- and post-MRI era with the cutoff in July 2014, when mpMRI was routinely incorporated into our AS protocol. Clinical outcomes were compared using Wilcoxon Rank Sum and Chi-square tests. Treatment-free survival was analyzed using Kaplan-Meier plots. A multivariable Cox regression analysis was performed to control for baseline characteristics.
Results: In total, 276 men were included in the MRI era versus 1015 in the pre-MRI era. There was no significant difference in baseline PSA (p=0.28) or Gleason Score (GS) (p=0.21). Men in the MRI era were more likely to discontinue AS (Figure 1) and had a shorter time to treatment (2.5 vs 5.9 years, P<0.001). At 2 years, 18% of men in the MRI era had undergone treatment as compared 10% in the pre-MRI era. On multivariable analysis, men in the MRI era experienced earlier disease reclassification even after controlling for baseline characteristics (P=0.003).
Conclusions: With widespread utilization of mpMRI, patients on AS are treated earlier. However, further follow up will be needed to see if this earlier identification and treatment of clinically significant disease ultimately results in a plateau in long-term treatment free survival. 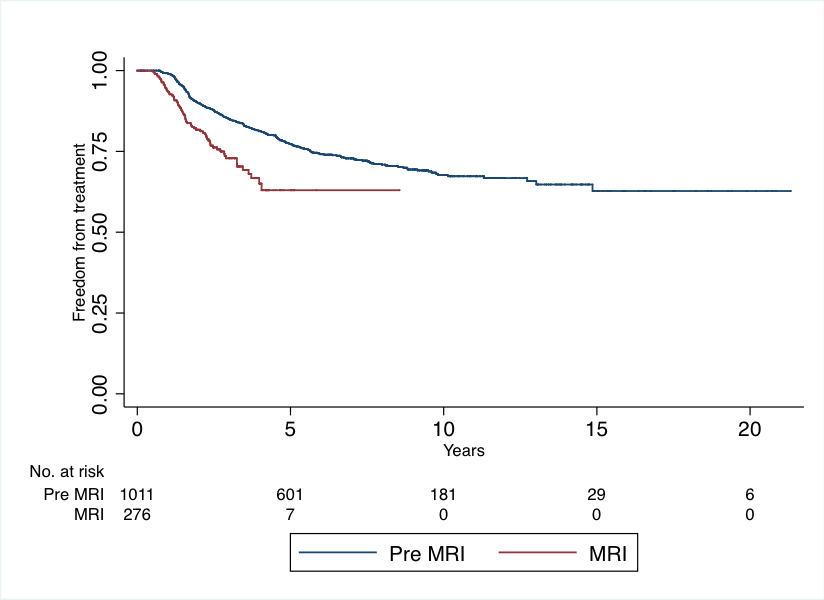
Back to 2019 Abstracts
