Clinical Utility of MR/Ultrasound Fusion-Guided Biopsy in Patients With PI-RADS 2 and 3 Lesions on Active Surveillance for Low Risk Prostate Cancer
Richard Ho, MD; Kamyar Ghabili Amirkhiz, MD; Michael S. Leapman, MD; Jeffrey C. Weinreb, MD; Peter G. Schulam, MD; PhD, Preston C. Sprenkle, MD
Yale School of Medicine, New Haven, CT
Background: Active surveillance has shown to a safe and effective management option for men with low-risk prostate cancer. Multiparametric magnetic resonance imaging (mpMRI) has demonstrated favorable performance in identifying occult high-grade cancers that would be missed on template biopsy alone. However, the utility of this approach in patients with low-suspicion lesions and otherwise low clinical risk is undefined.
Methods: We performed a retrospective analysis of 245 men undergoing active surveillance. Prostate Imaging Reporting and Data System (PI-RADS) version 2 was used to score regions of interest (ROI) on a scale of 1-5 corresponding to suspicion that clinically significant prostate cancer was present. PI-RADS scores 2 and above were targeted on biopsy. We identified 65 men (26.5%) whose highest suspicion lesion was PI-RADS 2 or 3. Clinically significant prostate cancer (csPCa) was defined as Gleason Score ≥ 3+4. We assessed the diagnostic accuracy of biopsy approaches using area under the receiver operator characteristic (ROC) curve and evaluated factors associated with csPCa in these patients using multivariate logistic regression.
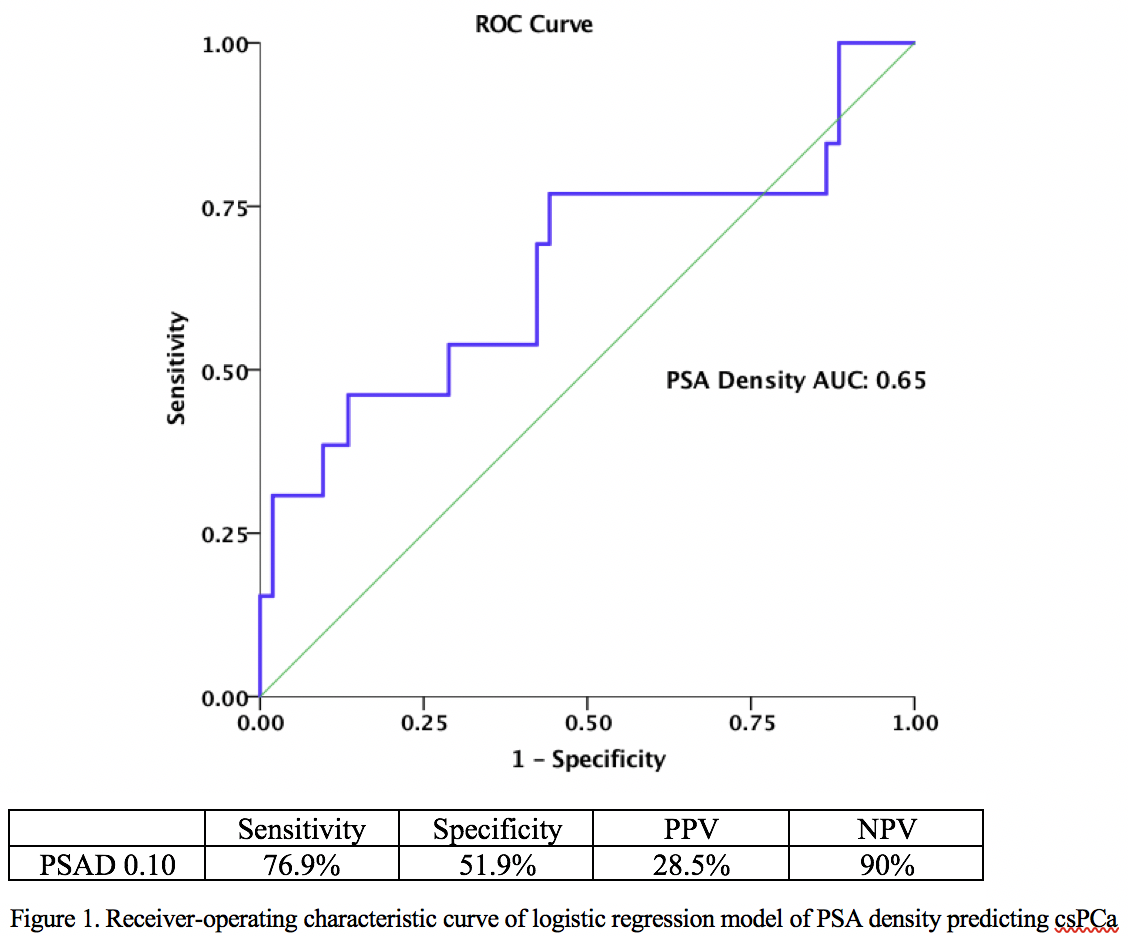
Results: CsPCa was identified in 13 of 65 patients (20%). These included five (38.4%) by systematic biopsy alone, six (46.2%) by targeted alone, and two (15.4%) by both approaches. On univariate analysis, the only significant variable predicting the detection of csPCa in men with low risk imaging mpMRI characteristics was higher PSA density (PSAD) (OR per 0.1 unit=2.18, 95% CI 1.14-4.16). A ROC curve of the logistic regression model of PSAD was performed (Figure 1). A PSAD cut-off of 0.1 resulted in a negative predictive value of 90%. When stratified by PI-RADS score with a PSAD cut-off of 0.1, a PI-RADS 2 score was associated with a sensitivity, specificity, PPV, and NPV of 66.6 %, 43.4%, 13.3%, and 90.9% respectively (AUC=0.55). A PI-RADS 3 score was associated with a sensitivity, specificity, PPV, and NPV of 80%, 58.6%, 40%, and 89.4% respectively (AUC=0.7).
Conclusion: In men with clinical low-risk prostate cancer on active surveillance with PIRADS 2 and 3 lesions, there is a low risk of upgrade to csPCa. Integration of PSA density may be a useful adjunctive tool in identifying patients at highest risk for upgrade despite favorable imaging findings. 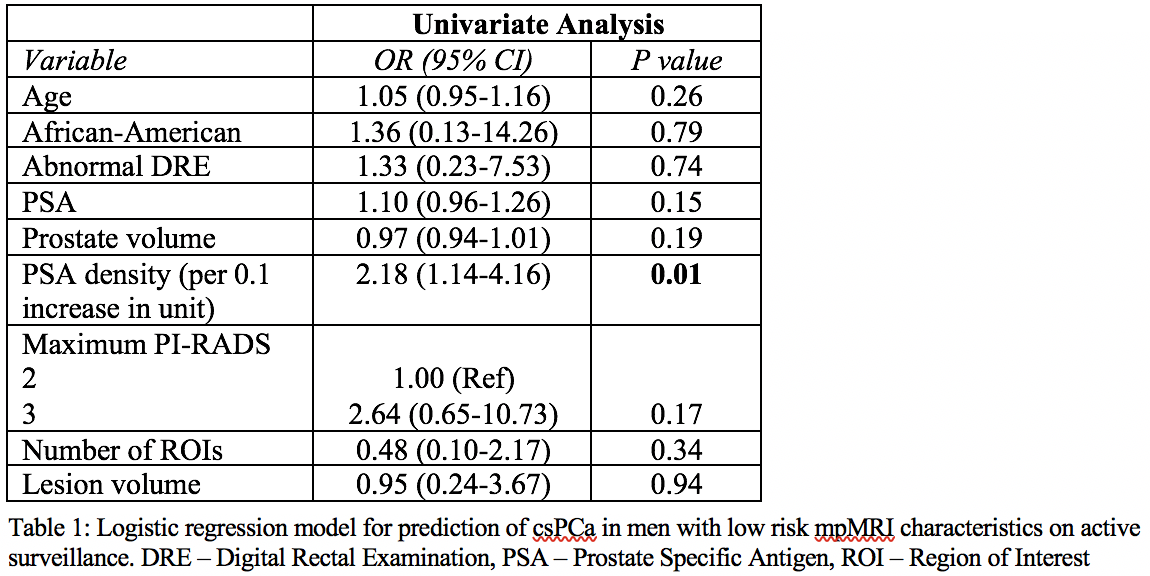
Back to 2018 Program
