Analysis of Urinary Extracellular Vesicles in Stone Formers Reveals Potential Target Proteins in the Formation of Nephrolithiasis
Ohad Kott, MD1; Jorge Pereira, MD1; Xuerong Wen, PhD2, Nagib Ahsan, PhD3; Jie Tang, MD4; Gyan Pareek, MD1
1Minimally Invasive Urology Institute, The Miriam Hospital, Providence, RI; 2University of Rhode Island, Kingston, RI; 3Department of Biology and Medicine, Brown University, Providence, RI; 4Rhode Island Hospital, Providence, RI
Introduction: Nephrolithiasis (NL) prevalence has increased 6 times in the last decade and is a tremendous burden on the healthcare system. The exact molecular pathophysiology of NL is unclear. Analysis of molecular components of kidney cells may help delineate the pathophysiology of NL. Extracellular vesicles (EV) are found in urine and contain peptides and other molecules. We studied urinary EV in various risk stone-formers in order to assess any differences in protein expression between non-, low- and high-risk (HR) stone formers.
Materials and Methods: Urine samples were collected from patients in our kidney stone center. Urine samples were classified as normal, low risk (LR) and HR stone formers. LR stone formers were patients with 1 stone episode and no recurrence. HR was defined as patients with stone burden >1cm, bilateral stone disease, or those with presentation at 18 years or younger. EV from urine samples were isolated and urine proteomes for each group were characterized using spectral counting mass spectrometry. Relative abundancy protein analysis for each of the groups was compared to analyze and difference in protein expression.
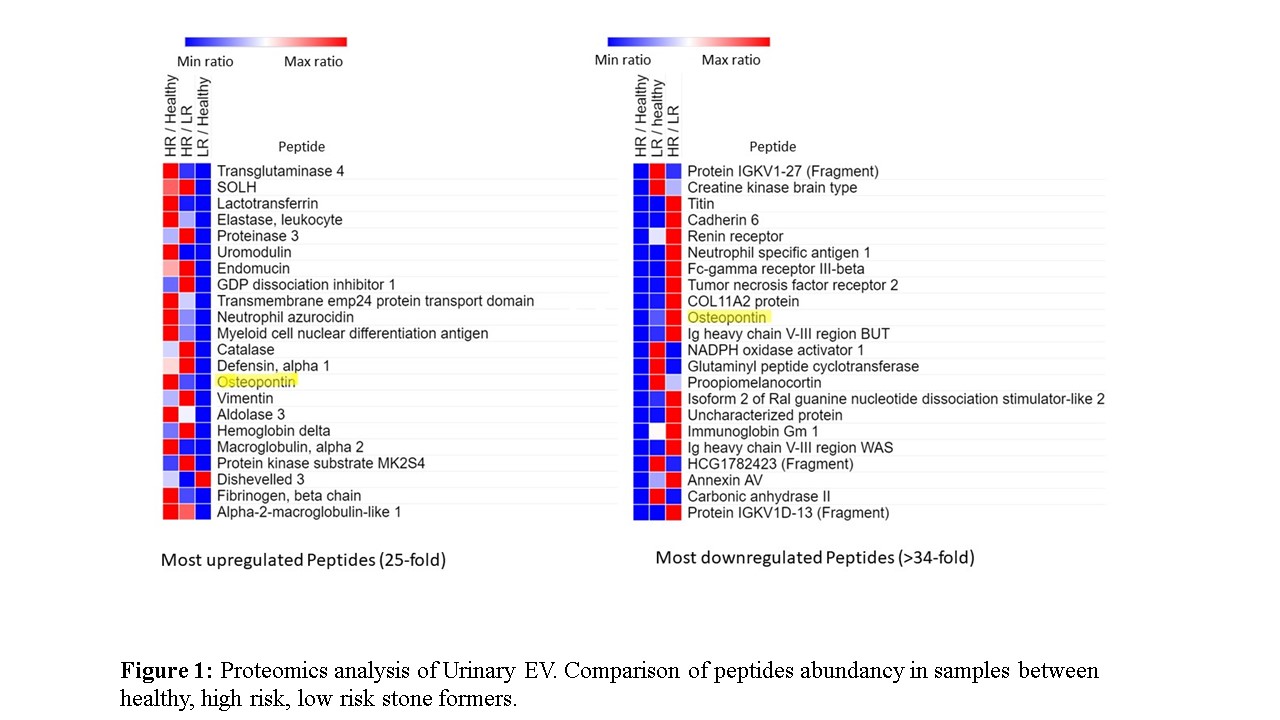
Results: 6 of 30 urines were available for analysis at the time of this report. Of these, 2 were from normal, 2 from LR and 2 from HR stone formers. A total of 1232 unique peptides were isolated and quantified in study samples. Comparative analysis revealed that 22 of these proteins have increased over 25 fold in stone formers compared to healthy individuals. Figure 1 shows these 22 most upregulated peptides (>25 fold) and the 22 peptides that were most downregulated (>34 fold) in HR and LR patients compared to the healthy samples.
Conclusions: A relative change in protein abundancy was observed in the cohort analysis. We demonstrate that proteins isolated from the EV of our population express proteins related to NL and the inflammatory response associated with NL. Additionally, we postulate that certain proteins (e.g Osteopontin) may be associated with mineralization and crystal formation and may be involved in kidney stone formation. The latter may serve as a target for further research to identify their exact pathophysiology of NL. A larger analysis is currently being conducted to validate the results.
Back to 2018 Program
