Heterogeneity in Early Oncologic Outcomes after Radical Prostatectomy in Men with National Comprehensive Cancer Network (NCCN) Intermediate-Risk Prostate Cancer
Kamyar Ghabili Amirkhiz, MD; Kevin Nguyen, MS, Amanda Lu, BA; Walter Hsiang, BS; Brian Shuch, MD; Michael Leapman, MD
Yale School of Medicine, New Haven, CT
Background
The National Comprehensive Cancer Network (NCCN) risk classification scheme for prostate cancer encompasses several definitions and has been shown to contain significant heterogeneity. Because patients possessing a single intermediate-risk feature may be regarded as ineligible for active surveillance, we aimed to compare pathologic and early oncologic outcomes between those with low-risk and intermediate-risk features based on the number of criteria met.
Methods
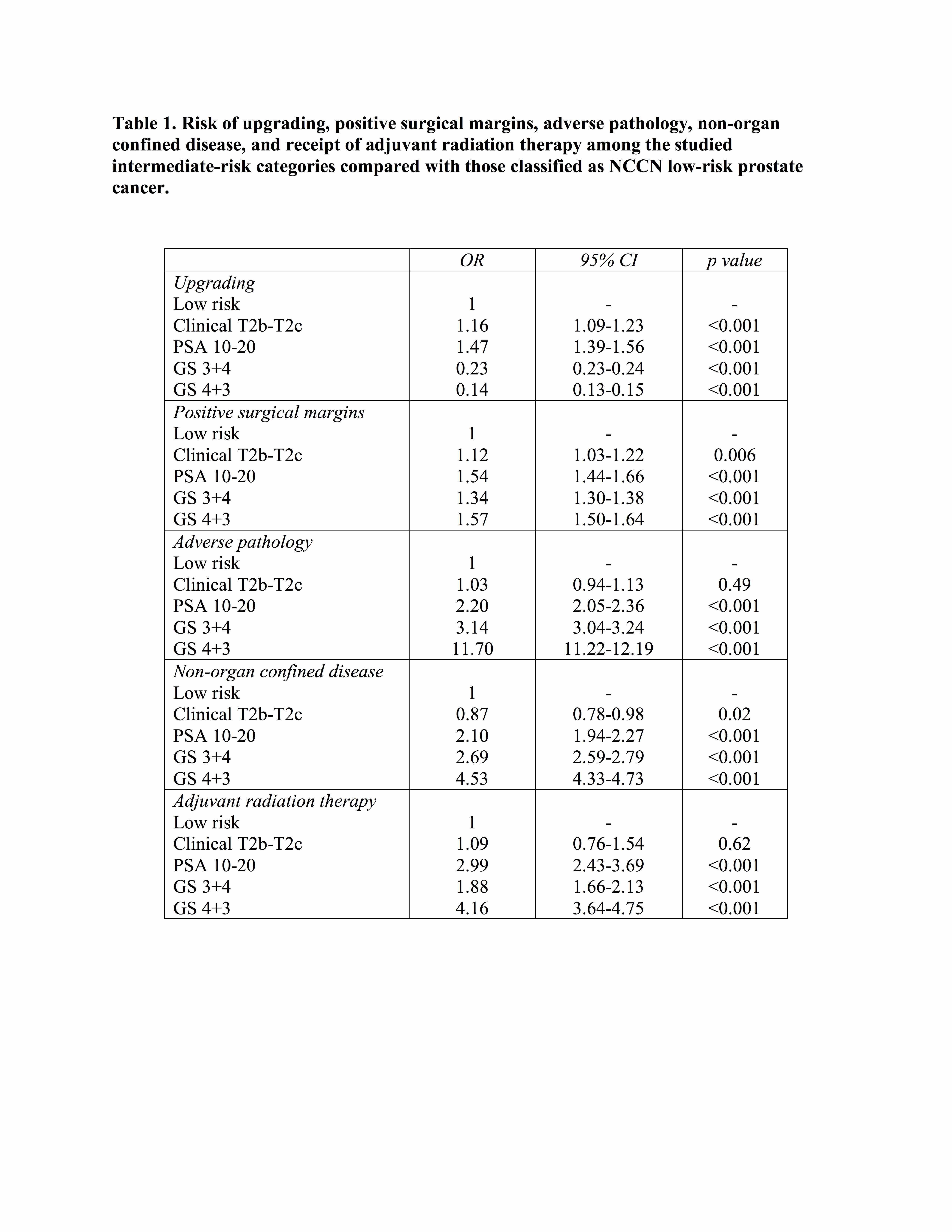
We queried the National Cancer Database (NCDB) to identify men with NCCN low-risk (cT1-T2a, prostate-specific antigen [PSA]<10 ng/mL, and Gleason score (GS)≤6) and intermediate-risk prostate cancer diagnosed from 2010-2014 who were treated with radical prostatectomy. Patients with intermediate-risk disease were stratified based on a single factor: clinical stage (cT2b-T2c), PSA (10-20 ng/mL), GS 3+4, or GS 4+3 alone (Figure 1). The pathologic outcomes including any Gleason upgrade, and adverse pathology (primary Gleason 4 or ≥T3 at radical prostatectomy), and receipt of adjuvant radiation therapy were compared between the low-risk and intermediate-risk groups. Odds ratios (OR) for pathologic outcomes and receipt of adjuvant radiation therapy were computed using logistic regression analyses.
Results
Of 181,847 patients treated with radical prostatectomy, we identified 30.7% and 37.1% with low-risk and intermediate-risk prostate cancer, respectively. Of 67,623 with intermediate-risk prostate cancer, 4,075 (6%) were due to clinical stage alone, 5,004 (7.4%) by PSA, 43,409 (64.2%) by GS 3+4, and 15,135 (22.4%) by GS 4+3 (Figure 1). Patients meeting intermediate-risk by clinical stage alone had similar risks of adverse pathology as low-risk patients (OR 1.03, 95%CI 0.94-1.13, p=0.49, Table 1). In contrast, those meeting intermediate-risk by PSA alone had higher risks of adverse pathology compared with low-risk individuals (OR 2.20, 95%CI 2.05-2.36, p<0.001, Table 1). Moreover, receipt of adjuvant radiation therapy was similar among low-risk and intermediate-risk patients by clinical stage alone (p=0.62), and higher among patients meeting definitions by PSA alone (OR 2.99, 95%CI 2.43-3.69, p<0.001, Table 1).
Conclusions
Based on national cancer registry data, early outcomes among men meeting the NCCN intermediate-risk definition for prostate cancer are heterogeneous. Intermediate-risk patients by clinical stage alone had similar rates of adverse pathology as did low-risk patients. Broadened eligibility for active surveillance should be considered to include those meeting favorable intermediate-risk definitions. 
Back to 2018 Program
