Predictors of Clinically Significant Prostate Cancer in Anterior Fibromuscular Stroma Lesions on Multi-Parametric Magnetic Resonance Imaging
Kamyar Ghabili Amirkhiz, MD; Richard Ho, MD; Michael Leapman, MD; Jeffrey Weinreb, MD; Peter Schulam, MD; PhD, Preston Sprenkle, MD
Yale School of Medicine, New Haven, CT
BACKGROUND
Multi-parametric magnetic resonance imaging (mpMRI) has been demonstrated to improve prostate cancer detection in anatomical areas previously difficult to sample on sextant biopsy alone, including the anterior fibromuscular stroma (AFMS). We aimed to investigate clinical and imaging parameters that may assist in identifying patients with AFMS lesions harboring clinically-significant prostate cancer (csPCa).
METHODS
We retrospectively queried our institutional mpMRI-ultrasound fusion biopsy database to identify patients with at least one region of interest (ROI) located in the AFMS on mpMRI who underwent fusion biopsy between March 2015 and December 2017 in the context of known or clinical suspicion of PCa. mpMRI findings were assessed, including prostate and ROI volumes, Prostate Imaging Reporting and Data System (PI-RADS) score, and location of the ROI (apex/midgland/base). Logistic regression and receiver operating characteristics curves with an area under the curve (AUC) were used to assess the ability of clinical and mpMRI characteristics to predict csPCa (Grade Group (GG) ≥2) in any core from a targeted biopsy of the ASMS lesion. Positive predictive value (PPV) for csPCa detection was also determined in each PI-RADS score.
RESULTS
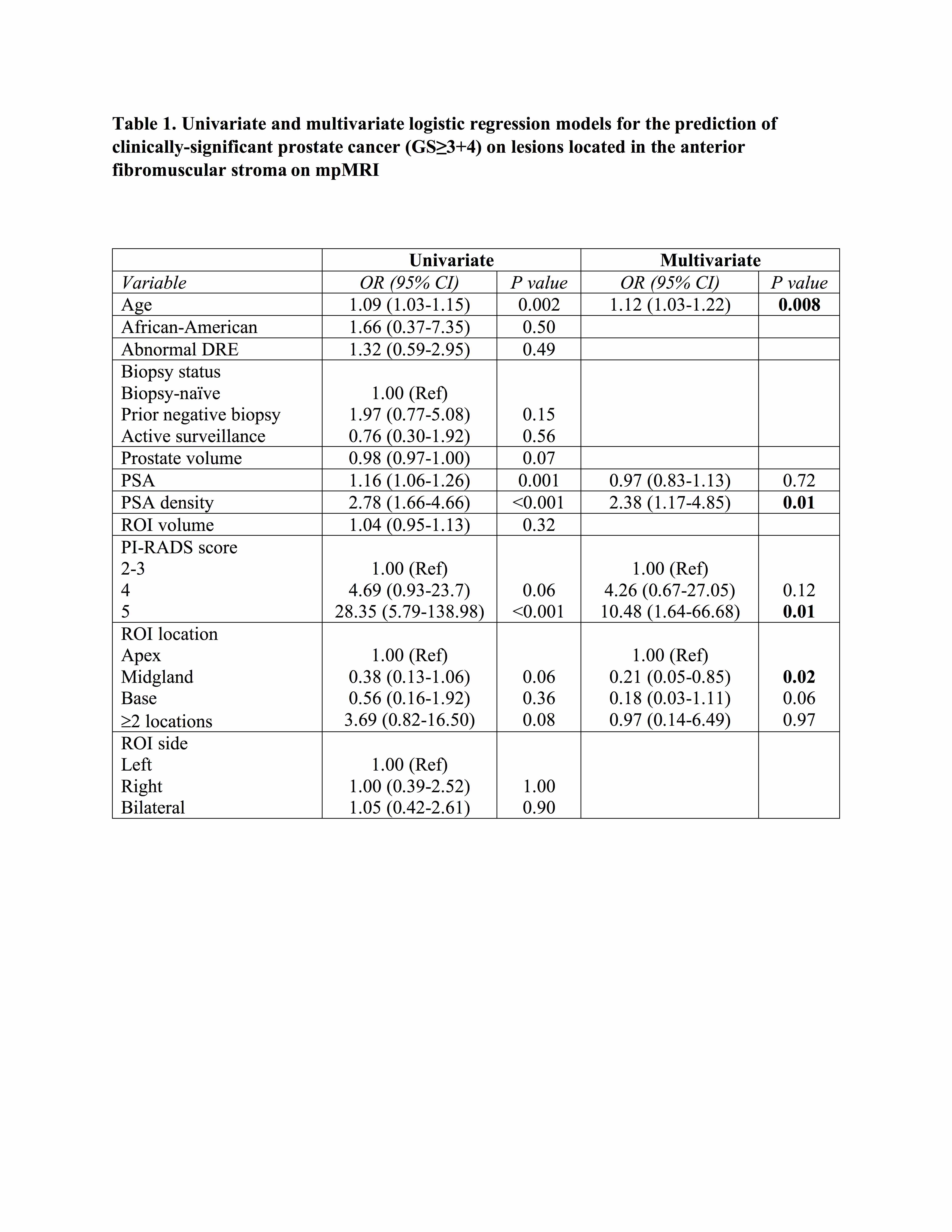
Of 756 men who underwent MRI-ultrasound fusion biopsy during the study period, 104 (13.7%) had at least one ROI in the AFMS. Of total 109 ROIs detected on mpMRI, 55 (50.4%) had csPCa and 18 (16.5%) showed perineural invasion on the biopsy of AFMS lesions. Detection of csPCa increased with the PI-RADS score (p<0.001, Figure 1). The PPV for csPCa detection of PI-RADS ≤3, 4, and 5 was 10%, 34.3%, and 75.9%, respectively. On multivariable analysis, older age (OR 1.12, p=0.008), higher PSA density (OR 2.38 per 0.1 increase in unit, p=0.01), higher PI-RADS score (5 vs 2-3, OR 10.48, p=0.01), and apical vs midgland location (OR 4.76, p=0.02) were associated with an increased likelihood of csPCa in AFMS lesions (Table 1).
CONCLUSIONS
AFMS lesions were identified in a minority of men undergoing mpMRI-ultrasound fusion biopsy. However, the targeted biopsy revealed csPCa in more than half of these patients. In patients with AFMS lesions on mpMRI, age, PSA density, PI-RADS score, and apical location are predictors of csPCa. 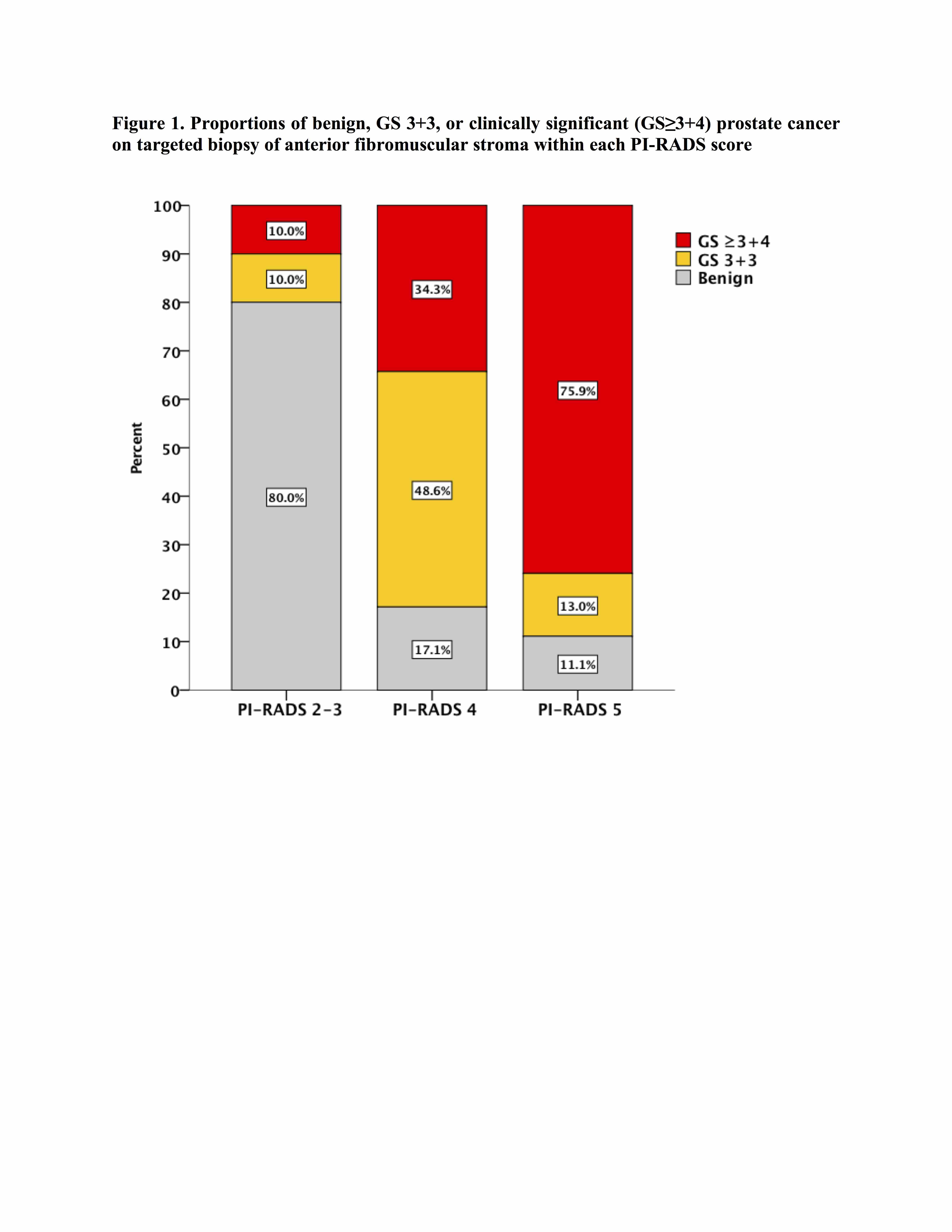
Back to 2018 Program
