Thirty Day Readmissions After Radical Cystectomy: Does the Hospital Make a Difference?
Alexander P. Cole, MD1; Sabrina Harmouch, MD1; Ashwin Ramaswamy, BA1; Phillip Gild, MD2; Stuart R. Lipsitz, ScD1; Mark Preston, MD1; Adam S. Kibel, MD1; Quoc-Dien Trinh, MD1
1Brigham & Women's Hospital, Boston, MA; 2Hamburg University Hospital, Department of Urology, Hamburg, Germany
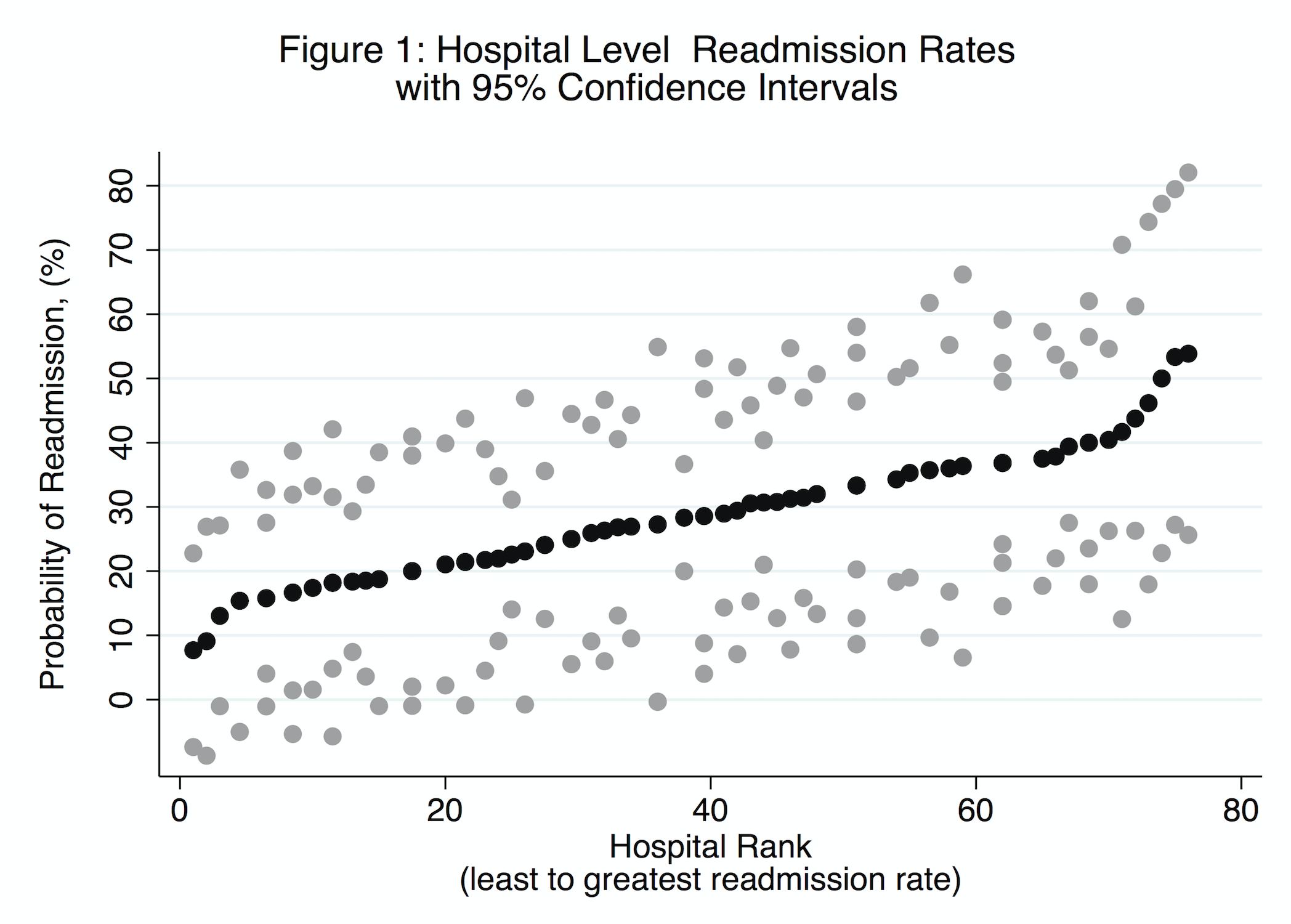
BACKGROUND: Hospitals are increasingly being held responsible for their readmissions rates. Some have questioned this, citing the large role of factors beyond the control of most hospitals. We designed a study to estimate the contribution of individual hospitals on the patient-level probability of readmission after radical cystectomyŚ a typical, complex cancer surgery.
METHODS: We utilized the Nationwide Readmissions Database (NRD), which is a large, nationally representative database designed for analysis of national readmissions rates including all payers and the uninsured. We identified all individuals who underwent radical cystectomy within the NRD during the first 11 months of 2014, survey weights were employed to generate national level estimates.The main outcome was readmission to any hospital within 30 days following an admission for radical cystectomy. Using a multilevel mixed effects model, we estimated the influence of hospital and clinical variables on patients' probability of readmission. A hospital-level random effects term was used to estimate the contribution of each hospital to their patients' probability of readmission.
RESULTS: We identified a weighted sample of 6,808 individuals who received radical cystectomy at 341 hospitals in the United States. The 30-day readmission rate was 29.7% (95% CI 28.0 - 31.4). In our adjusted model, female sex and comorbidity score were associated with increased likelihood of readmission, however hospital characteristics such as bed size and surgical volume were not. Individual hospitals did not meaningfully contribute to the model for readmission (pseudo R-squared < 0.01%).
CONCLUSIONS: After adjusting for patient level characteristics, the hospital where surgery was performed did not meaningfully add to a model predicting patient-level probability of readmission. Our findings underscore the potential limitations of using 30-day post-discharge readmissions as a hospital metric. 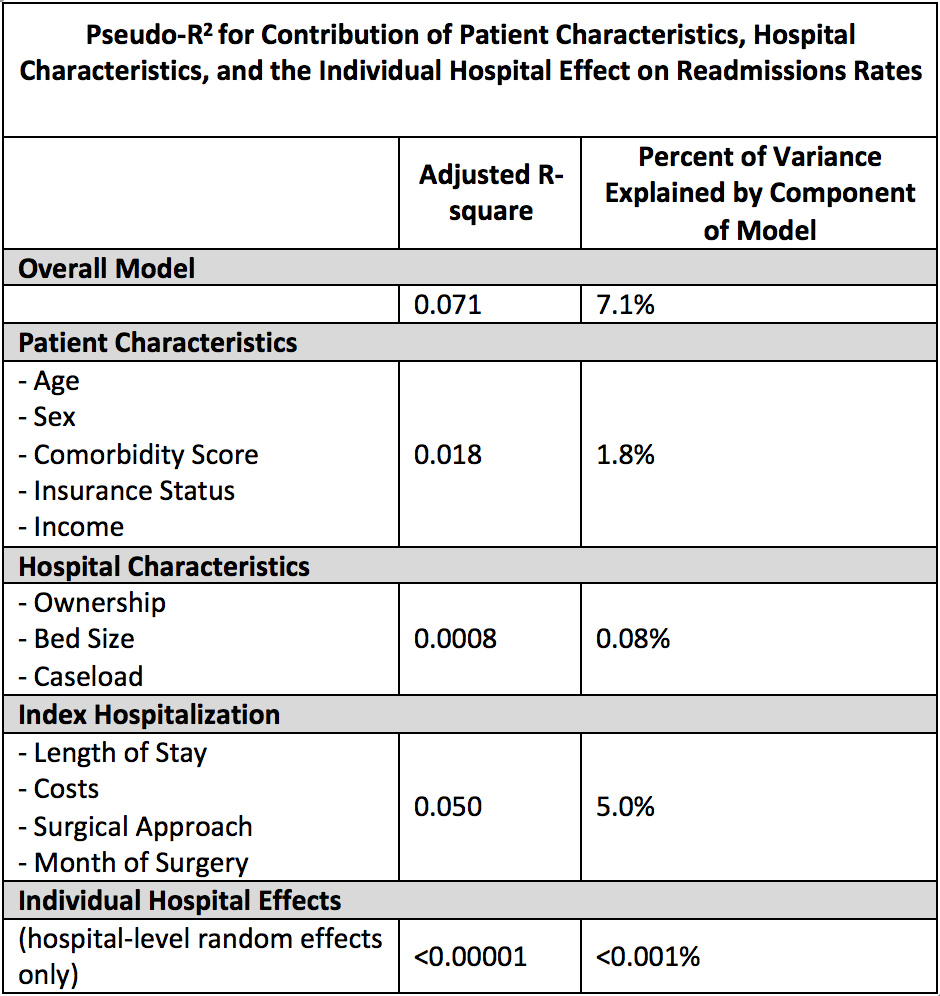
Back to 2018 Program
