Positive Surgical Margins Following Robotic Prostatectomy: Should Location be Considered in Planning Further Treatment?
Jacob Baber, MD; Ilene Staff, PhD, Tara McLaughlin, PhD, Joseph Tortora, MS; Joseph Wagner, MD
Hartford Hospital, Hartford, CT
Background: Following prostatectomy for prostate cancer, the importance of the location of a positive surgical margin (PSM) as a guide to further disease management is not well understood. Here we evaluated the degree to which location of PSM following radical prostatectomy for prostate cancer was associated with recurrence (surgical failure).
Methods: We performed a retrospective review of a prospectively maintained database of patients who underwent a robotic-assisted laparoscopic radical prostatectomy (RALP) between January 2004 to December 2016 to identify those who had a PSM on final pathology. Margins were categorized based upon location. Those described in only one region (i.e., apical, posterior, anterior, base, lateral, mid) were categorized as "pure"; those described as occurring across regions (e.g., posterior-lateral and posterior-mid) were placed into "mixed" categories. Multiple PSM in different regions (e.g., apex and base) were excluded from the mixed category. Patients with margins in each location were compared to all others on surgical failure (SF; defined as PSA > 0.2 ng/ml), salvage treatment after a pattern of rising PSA not reaching 0.2, or persistent disease (never below .2). To evaluate time to recurrence and account for any difference in opportunity to recur (follow-up time), a Kaplan Meier (KM) analysis was conducted on each of the comparisons. After Bonferroni correction, a p value of .005 was considered significant for each test.
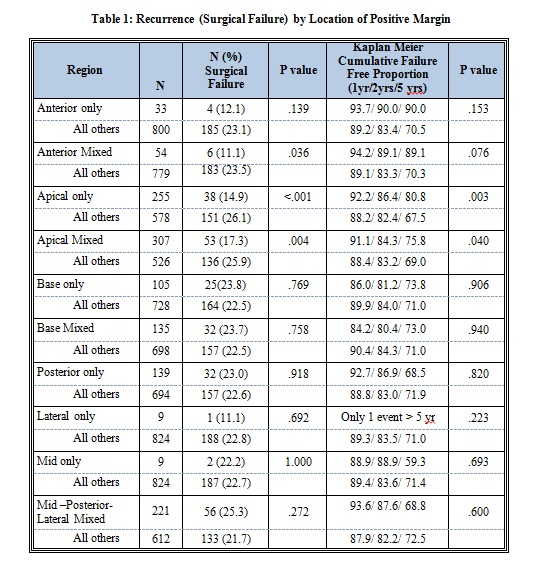
Results: Of 3950 patients who underwent RALP, 880 (22.3%) had a PSM. Post-operative PSA was available for 833 men comprising the analytic dataset. Median follow-up was 41 months. Of the 833 men included in the analysis, SF occurred in 22.7% of patients overall. The pure apical and mixed apical groups were less likely to have SF than the comparison groups (p <.001 and p = .004, respectively); the mixed anterior group was also less likely to experience SF but this did not reach the corrected significance level established above. KM indicated that patients with pure or mixed apical margins had significantly longer time to failure (Table 1).
Conclusions: PSM at any location involving the apex was associated with more positive outcomes relative to other locations. Location of PCM should be considered when planning treatment after RALP.
Back to 2018 Program
