Trends in Regional Narcotic and NSAID Use in Emergency Department Patients with Acute Renal Colic
Alexandra Berger, MD1; Ye Wang, PhD1, Benjamin Chung, MD2; Steven Chang, MD1; George Haleblian, MD1
1Brigham and Women's Hospital/Harvard University, Boston, MA; 2Stanford University, Palo Alto, CA
BACKGROUND: Since 1999, the rate of fatal prescription drug overdoses in the United States has nearly quadrupled. A national effort to decrease opiate administration has been undertaken. This study examines the trends in narcotic and ketorolac administration in the Emergency Department amongst patients presenting with a diagnosis of acute renal colic.
METHODS: We identified all individuals presenting to the Emergency Department with a primary diagnosis of urolithiasis (ICD9 592.0, 592.1, 592.9, 274.11) from 2006-2015 in the Premier Hospital Database, a nationally representative discharge database. To focus on non-toxic patients, we limited our cohort to patients with the following criteria: discharge in one day or less, no intravenous antibiotics, no admission to the ICU, no procedures, and no inpatient mortality; we also excluded patients with a history of chronic pain syndrome and renal insufficiency. We then assessed for trends in the receipt of narcotic pain medication, based on morphine equivalents, and ketorolac, through multivariable regression models adjusting for patient and hospital characteristics.
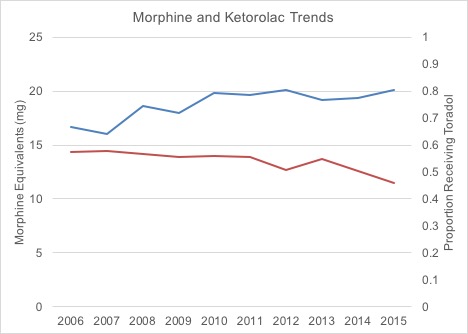
RESULTS: The total amount of morphine received by renal colic patients in the Emergency Department increased from 16.7 milligrams in 2006 to 20.1 milligrams in 2015 (Figure 1). Over this same time, the percentage of all patients receiving ketorolac decreased from 57.3% to 46.0% (Figure 1). There was an increased utilization of narcotics in the Midwest (14.5 to 17.6 milligrams), Northeast (16.0 to 18.3 milligrams), and South (15.6 to 19.6 milligrams) regions over time. The West region's median narcotic utilization was stable (25 milligrams) but higher than the other regions.
CONCLUSIONS: Over the study period, patients received higher amounts of morphine during encounters in the Emergency Department for acute renal colic. In this same period, fewer patients were given ketorolac. This study demonstrates that despite a national movement to reduce the use of opiate pain medications in favor of non-narcotic agents, patients presenting with acute pain due to renal colic receive more opiates in the Emergency Department now than a decade ago.
Back to 2018 Program
