Complications and Survival of Primary Cystectomy, Primary Cystectomy with History of Pelvic or Abdominal Radiation and Salvage Cystectomy after Trimodality Therapy
Alberto Pieretti, MD; Ross Krasnow, MD; Naren Nimmagadda, MD; Adam Feldman, MD MPH; Matthew Wszolek, MD
Massachusetts General Hospital, Brookline, MA
BACKGROUND: Trimodal therapy (TMT) involving transurethral resection of bladder tumor, external beam radiation and chemotherapy has become an acceptable option for treatment of muscle invasive bladder cancer. Salvage cystectomy is reserved for those patients who fail bladder preservation by TMT. We compared complications and survival outcomes between primary cystectomy (PC), salvage cystectomy (SC) and primary cystectomy with prior history of abdominal or pelvic radiotherapy (PC+XRT).
METHODS:
Two hundred and seventy-five patients were identified and retrospectively reviewed who underwent radical cystectomy at Massachusetts General Hospital for clinical cT1-T4 disease between 2003 to 2013. Patients who underwent radical cystectomy for benign or clinical cT0, cTa, or cTis disease were excluded. Patients were grouped as having PC with or without neoadjuvant chemotherapy, SC, or PC+XRT. Early complications (≤90 days) and late complications (>90 days) were compared between surgical groups by organ system and Clavien-Dindo classification. Disease-specific survival (DSS) and overall survival (OS) were evaluated between surgical groups using the Kaplan-Meier method.
RESULTS: The incidence of any early complication for PC, SC and PC+XRT were 60.1%, 76.1% and 61%, respectively (p=0.36). Early respiratory, infectious and neurological complications were more common in SC than in PC or PC+XRT (respiratory: 19.0%, 5.0%, 14%, respectively; p=0.01) (infectious: 38.1%, 17.1%, 7%, respectively; p=0.02) (neurological: 23.81%, 5.5%, 0%, respectively; p=0.007). The rate of early significant complications as defined by Clavien-Dindo grades 3-5 was 27.7% for PC, 33.3 % for SC and 21.4% for PC+XRT (p= 0.6). Late complications are more common in SC compared to PC and PC+XRT (57.1%, 21.3%, 36%, respectively, p=0.002). Higher incidence of late infectious, gastrointestinal and genitourinary complications was seen in SC compared to PC and PC+XRT (Infectious 23.8%, 7.4 %, 11%, respectively; p=0.03) (gastrointestinal 23.8%, 4.1%, 14%, respectively; p= 0.001) (genitourinary 24%, 7.8%, 1%; p=0.03). The rate of significant late complications graded Clavien-Dindo 3-5 was 52.3% for SC, 2.6% for PC and 35.7 % for PC+XRT (p=0.008). DSS at 5 years after surgery was 63.8% for SC, 63% for PC and 61.1 for PC+XRT (p=0.9). OS at 5 years after surgery was 29% for SC, 47.8% for PC and 45.5% for PC+XRT (p=0.8).
CONCLUSIONS: SC is associated with higher incidence of any and significant late complications. SC was associated with higher incidence of early respiratory, infectious and neurological complications; and late infectious, gastrointestinal and genitourinary complications. SC after TMT does not represent a delay in treatment since DSS and OS from the time of surgery are similar between the 3 groups. 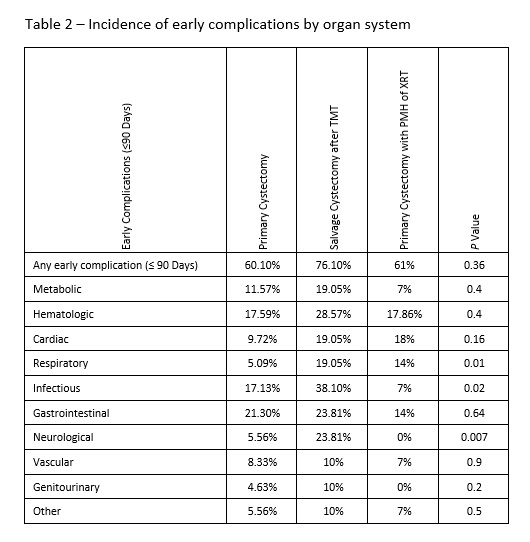


Back to 2018 Program
