Factors Associated with Readmissions after Radical Cystectomy
Christine Cumarasamy-White, MD; Jacob Baber, MD; Ilene Staff, PhD, Kevin Pinto, BS; Joseph Tortora, MS, Tara McLaughlin, PhD, Mika Gauger, BS; Akshay Gangakhedkar, BS; Anoop Meraney, MD
Hartford Hospital, Hartford, CT
Introduction: Radical cystectomy (RC) is the standard of care treatment for muscle-invasive bladder cancer. This major surgical procedure is associated with a high readmission risk. Here we sought to identify demographic, clinical and perioperative factors that are associated with readmission after RC.
Materials and methods: We retrospectively reviewed our bladder cancer database to identify patients who were diagnosed with primary bladder cancer and treated with RC from January 1, 2007 through September 30 2017. A series of univariate analyses (Chi square or Wilcoxon signed rank test, as appropriate) identified demographic, clinical, and operative factors that were significantly associated with 30 day and 90 day readmission after RC, respectively. A p value of <.05 was then used as the cut off for inclusion in multivariate logistic regression.
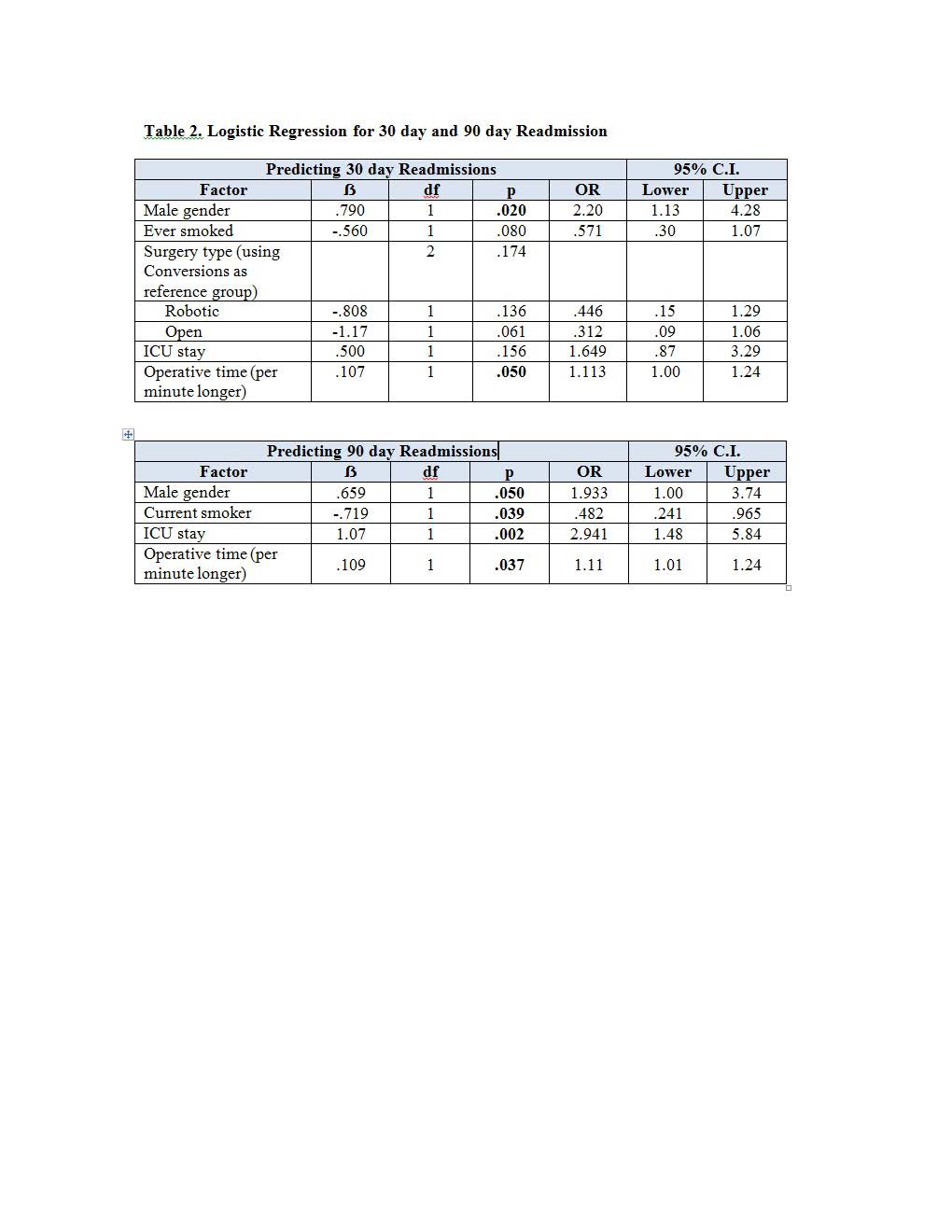
Results: A total of 283 patients (232 men, 51 women) had RC at our institution during the study period. The median (IQR) age was 69 (62.0, 76.0) and median (IQR) BMI was 27.1 (24.2, 30.2). Most (69.6%) had robotic surgery, 19.4% had open and 11.0% converted to open. Readmission rates at 30 and 90 days were 31.6% and 39.2% respectively. Table 1 presents associations between demographic, clinical, and operative factors and 30 day and 90 day readmissions. Females were more likely to be readmitted at both time points (p = .01 and .03 for 30 and 90 day readmissions, respectively). Similar results were observed for those with longer operative times (p = .018 and .016, for 30 and 90 day readmissions, respectively). Patients who were readmitted at both time points were more likely to have been in the ICU (p = .047 and .001 for 30 and 90 day readmissions, respectively). Logistic regression (Table 2) indicated that male gender, smoking status, OR time and ICU were significantly associated with readmission. ICU stay and operative time were both associated with increased risk of readmission at 90 days.
Conclusions: Readmission following RC remains a major concern. In this study we identify risk factors associated with readmissions following RC. Quality improvement projects can be aimed toward targeting these risk factors in order to reduce the readmission risk. 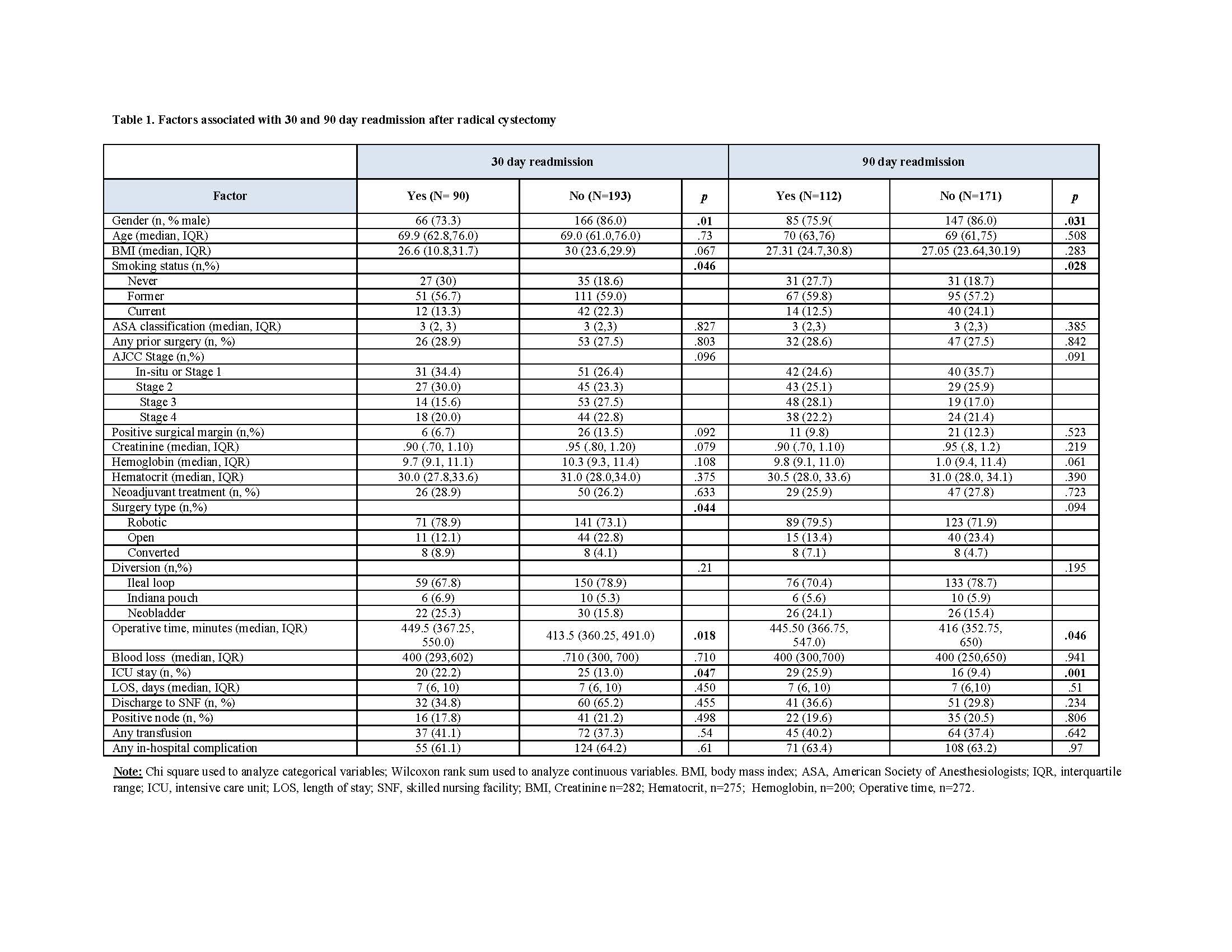
Back to 2018 Program
