Concurrent Urologic Surgeries Increase the Risk of Infection: A National Database Study
Valary T. Raup, MD1; Ramy Abou Ghayda, MD1; Abraham Chiang, MD1; Julie Szymaniak, MD1; Steven L. Chang, MD1; Benjamin I. Chung, MD2; Martin Kathrins, MD1
1Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 2Stanford Medicine, Palo Alto, CA
BACKGROUND: Surgical infections are a vexing problem that put significant strain on our healthcare system. There have been multiple studies looking at infection rates after various solo urologic surgeries. We sought to examine the rates of postoperative infection when endoscopic surgery is performed concurrently with another type of urologic surgery using a large national database.
METHODS: The Premier Hospital Database (2003-2015) was queried using International Classification of Diseases (ICD-9) procedural codes (CPT) codes for urologic procedures split into 7 categories: endoscopic, urethral, scrotal, testes, penile, implants, spermatic cord/vas. Endoscopic procedures were run against the other 6 categories of urologic surgery. Infection rates were evaluated divided into subcategories of soft tissue infection (STI), sepsis, clostridium difficile (C. diff), urinary tract infection (UTI), pneumonia, and other infections. We assessed for a relationship between the type of concurrent procedure and infection, adjusting for patient and hospital characteristics.
RESULTS: A total of 487,725 patients were identified to have undergone endoscopic procedures, 2.7% of which also underwent a concurrent urologic procedure (n=13,546). The most common concurrent procedure was urethral (86%), followed by penile procedures (8%), scrotal and implant procedures (2% each), and seminal vesicle/vas procedures (1%). Concurrent urologic surgery was associated with Caucasian race (75%, p<0.001), male gender (79%, p<0.001), marriage (62%, p<0.001), Charleston Comorbidity Index 0-1 (63.5%, p<0.001), Medicare payor (62%, p=0.046), non-teaching hospitals (68%, p<0.001), smaller hospitals (p<0.001), and being in the Midwest region (p<0.001). Accounting for patient/hospital factors, urethral and penile procedures were strongly associated with increased rates of overall infections and UTIs, while scrotal procedures were strongly associated with STI and implant procedures were strongly associated with other infections not specifically characterized (all p<0.0001) (Table 1).
CONCLUSIONS: Concurrent urologic surgery is uncommon but associated with increased infection rates. Further studies are needed to better delineate how we can tailor our clinical practices and antibiotic choice to better prevent these infections. 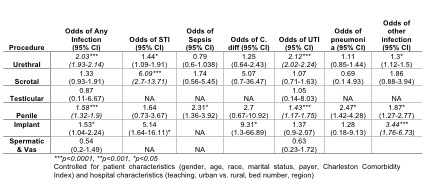
Back to 2018 Program
