Operating Room Efficiency Improves with Increasing Staff Experience and Structured Pre-operative Briefing
Adam Ludvigson, MD; Christina Gentile, MPH; Johann Ingimarsson, MD
Maine Medical Center, Portland, ME
BACKGROUND: Surgical procedures can vary greatly in complexity and equipment needs. Compared to other endoscopic procedures, for example, percutaneous nephrolithotomy (PCNL) requires a much larger and more varied set of equipment, which presents unique challenges to the surgeons and OR staff. This can lead to more time in the OR spent not performing the actual procedure, but rather setting up equipment, positioning the patient, and other non-operative tasks. Our study used this procedure to examine whether OR time was more efficiently used when staff was formally briefed on the upcoming case, and when a more experienced OR team was present.
METHODS: Beginning in December 2016, OR staff were included on a briefing email sent the night before each PCNL detailing the surgical plan, anticipated equipment needs, and any other challenges likely to arise during the case. An Epic report was generated containing time in room, time of actual procedure, and OR staff present for all PCNLs performed during a 2-year period spanning this intervention. Non-operating time (NOT) was defined as the difference between the duration of time in the room and the duration of the procedure itself. The level of experience amongst the staff for any given case was determined by averaging the number of PCNLs each staff member had participated in during the examined time period. Statistical analysis was performed with IBM SPSS Statistics version 23.
RESULTS: During the examined time period, 104 PCNLs were performed. Prior to the regular briefing email, average NOT was 58.6 minutes, which decreased to 49.5 minutes afterwards (p < 0.01). Plotting NOT per average number of cases performed by staff revealed a significant negative association, with increasing OR staff experience leading to shorter NOT (r=-0.35, p < 0.01).
CONCLUSIONS: Initiating regular pre-op communication with OR staff modestly but significantly reduces time in the room relative to the procedure itself. Crucially, more experienced OR teams were associated with significantly less time in the operating room spent not performing the procedure itself. Though our analysis only included one type of procedure, these findings demonstrate that efficiency is demonstrably improved with better communication and more experienced staff, which is potentially generalizable to any complex surgical procedure. Simple interventions, such as a briefing email, should be combined with careful attention to OR staff experience to maximize OR efficiency and patient safety. 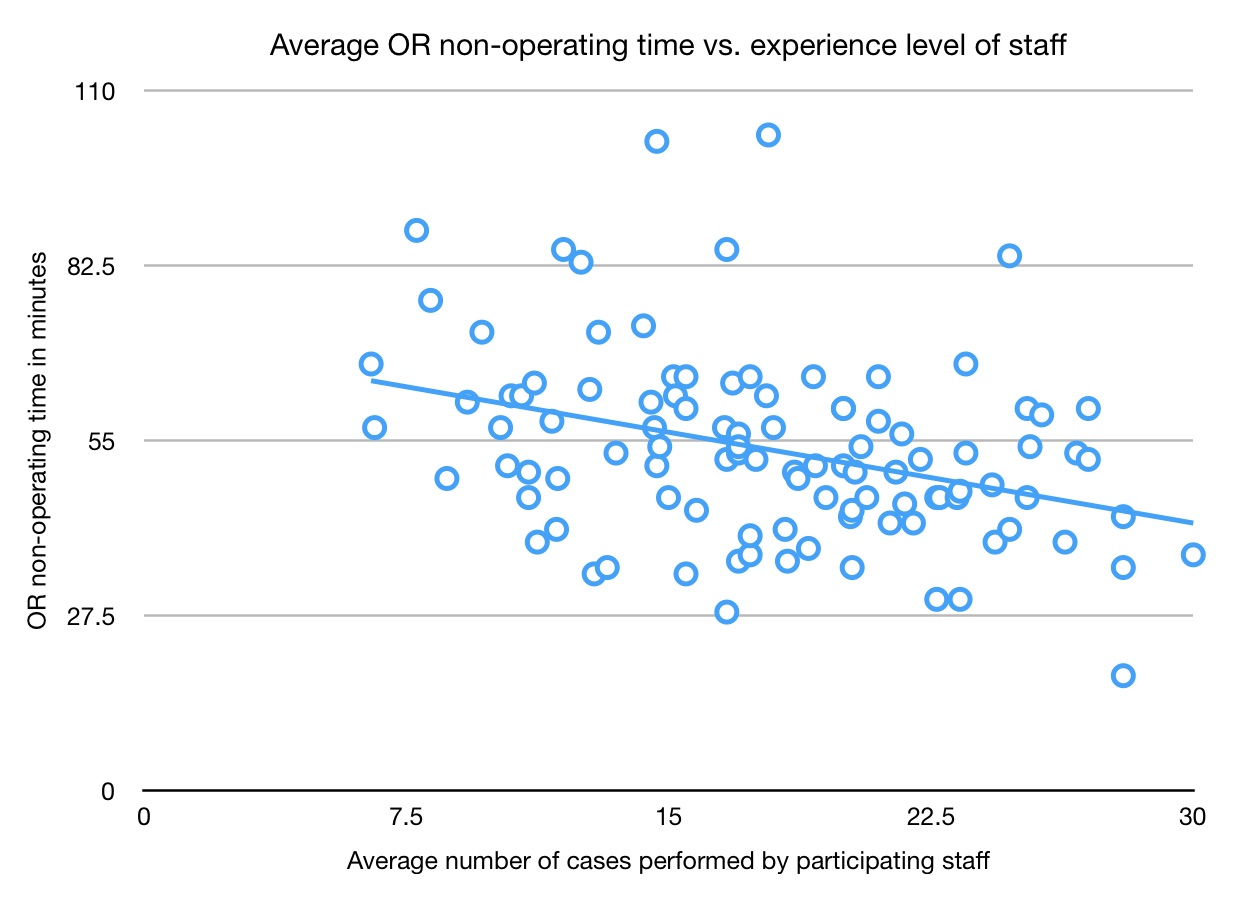
Back to 2018 Program
