Analyzing the Cost-Effectiveness of Six Therapies for Treating Lower Urinary Tract Symptoms Due to Benign Prostatic Hyperplasia
Andrew J. Tompkins, MD1; James C. Ulchaker, MD2; Melissa S. Martinson, PhD3.
1Brown University, Providence, RI; 2Cleveland Clinic, Cleveland, OH; 3Technomics Research, Minneapolis, MN
Introduction: To conduct a cost-effectiveness analysis from payers' perspectives of six treatments for lower urinary tract symptoms (LUTS) due to benign prostatic hypertrophy (BPH) and to examine these modalities in the marketplace for the best use of healthcare funds and quality of life benefits for patients.
Methods: The economic analysis was conducted with a Markov model to compare combination drug therapy (ComboRx), minimally invasive procedures (MITs) - water vaper thermal therapy (Rezūm), conductive RF thermal therapy (Prostiva) and prostatic urethral lift (UroLift), and invasive surgical procedures - photovaporization of prostate (Greenlight PVP) and transurethral resection of the prostate (TURP). Effects were assessed based on the average changes in the International Prostate Symptom Score (IPSS) with treatment effects modeled using a common IPSS baseline score. Adverse events and retreatment rates were estimated from medical literature. Starting with each therapy, patients' transitions to more intensive therapies when symptoms returned were simulated in 6 month cycles over 2 years. Incremental cost-effectiveness ratios (ICERs) were calculated for pairs of treatments; uncertainty in ICERs estimated with probabilistic sensitivity analyses.
Results: ComboRx was least effective and provided one-third of the symptom relief achieved with MITs. UroLift was similar in effectiveness to Prostiva and Rezūm but costs more than twice as much. The cheaper MITs were about $900 more expensive than ComboRx generic drugs over 2 years. TURP and PVP, typically reserved for treatment of more severe LUTS, provided slightly greater relief of LUTS than MITs at about twice the cost over 2 years.
Conclusions: The analysis evaluated the costs and symptom relief of six treatment options in the continuum of care from a common baseline of LUTS severity. Identification of treatments for LUTS/BPH that demonstrate cost-effectiveness and provide appreciable symptom relief is paramount as reimbursement for patient care moves from volume-based services to value-based services.
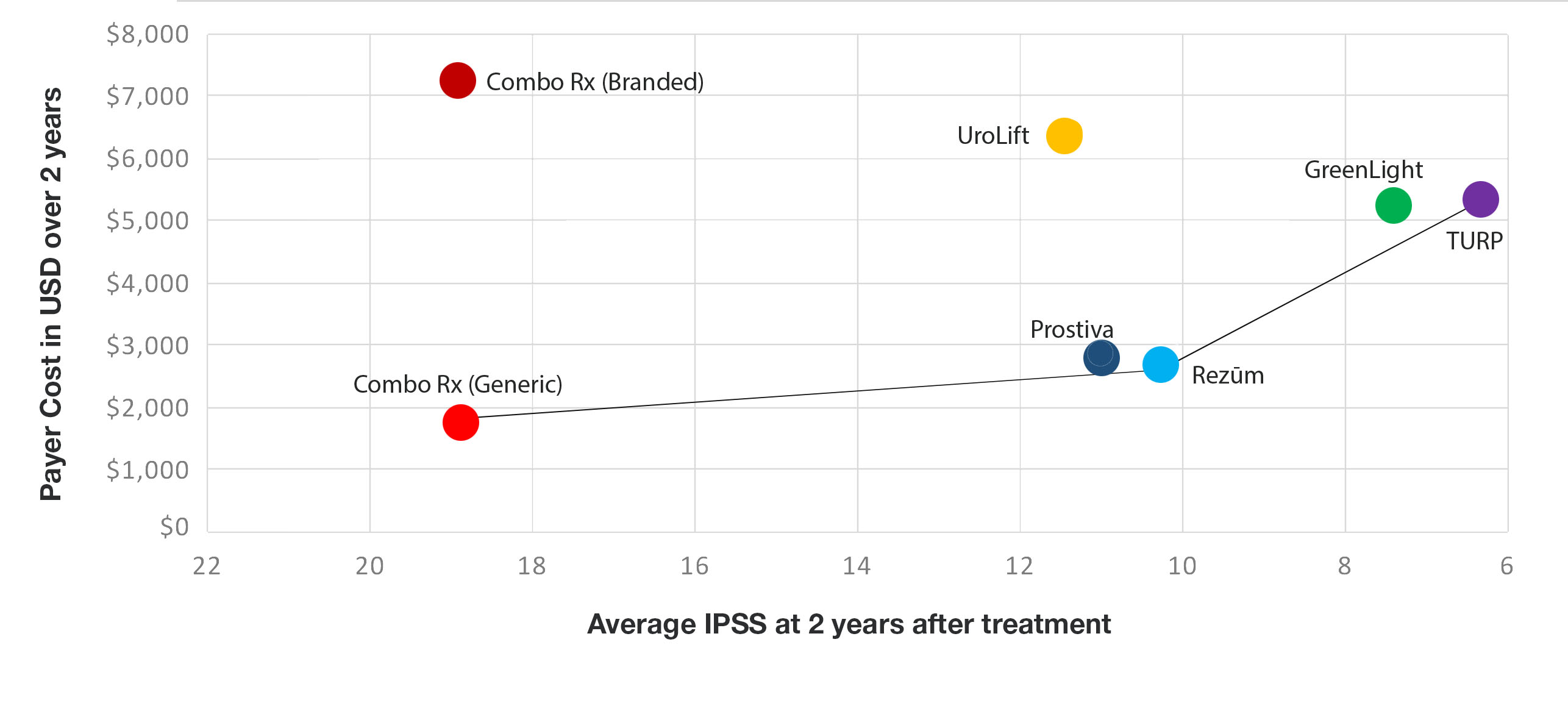
Fig. Therapies along the line represent the most efficient treatments, i.e. those with greater symptom relief for the money spent.
Back to 2018 Program
