Long-term Oncologic Comparison of Radiofrequency Ablation to Partial Nephrectomy for T1 Renal Cell Carcinoma using Propensity Score Analysis
Naren Nimmagadda, MD1; Yichuan G. Hsieh, PhD1; David Kuppermann, MD1; Michael Grant, MD1; Sarah Psutka, MD2; Christopher B. Allard, MD3; Francis McGovern, MD1; Douglas Dahl, MD1; Michael Blute, MD1; Ronald Arellano, MD1; Debra Gervais, MD1; Adam Feldman, MD; MPH1
1Massachusetts General Hospital, Boston, MA; 2Northwestern University Feinberg School of Medicine, Chicago, IL; 3McMaster University, Hamilton, ON
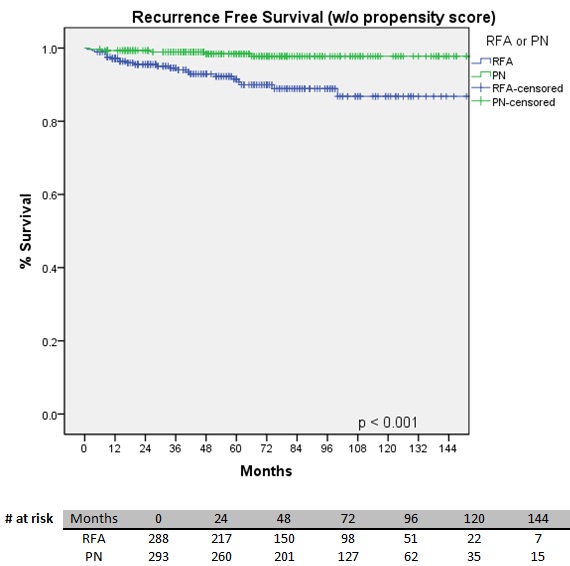
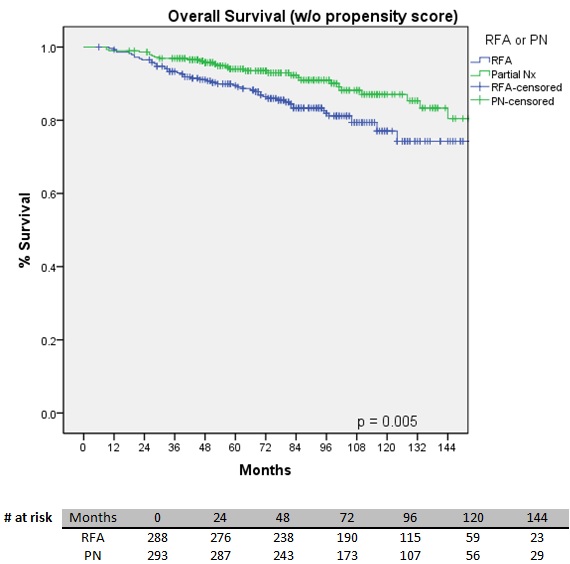
BACKGROUND: Radiofrequency ablation (RFA) of clinical T1 (cT1) renal cell carcinoma (RCC) is a well-established option. Comparisons to partial nephrectomy (PN) in similar patients are infrequently reported due to significant differences in age and comorbidities. Our objective is to compare oncologic outcomes after RFA to those for PN for treatment of sporadic, cT1 RCC in a large cohort with strict exclusion criteria using propensity score analysis to reduce the effect of confounding variables. METHODS: All patients (n = 1,255) who underwent RFA or PN at a single institution between 1998-2014 were retrospectively reviewed. Only solitary cT1 lesions, proven as RCC on pre-RFA biopsy or surgical pathology, were included. Exclusion criteria were prior RCC, RCC-associated genetic syndrome, > 1 lesion, metastasis at presentation, follow-up < 6 months, and/or metachronous tumor development. Residual disease after RFA was defined as enhancement on initial post-RFA imaging. Local recurrence was defined as enhancement after initially negative post-procedure imaging, and was carefully discriminated from metachronous tumor development. A propensity score was calculated using a binary logistic regression including age, Charlson score, and location (R.E.N.A.L. score). Patients were stratified and compared by quintiles of the propensity score. Recurrence-free (RFS), metastasis-free (MFS) and overall survivals (OS) were estimated using the Kaplan-Meier method before and after stratification. The log-rank test was used to assess differences in survival and was pooled to assess significance across quintiles. RESULTS: 288 RFA and 293 PN patients were included. Only age, Charlson score, and location (R.E.N.A.L. score) were significantly different between groups with no significant difference in clinical stage or total R.E.N.A.L. score. Median oncologic follow-up was 53 months after RFA versus 65 months after PN. RFA patients experienced 23 recurrences, 13 metastases, and 54 deaths while PN patients experienced 6 recurrences, 7 metastases, and 30 deaths during follow-up. RFA patients had significantly worse RFS (p < 0.001) and OS (p = 0.005) than PN patients by Kaplan-Meier estimates while metastasis-free survival (MFS) was not significantly different (p = 0.081). After stratifying by propensity score, there remained a significant difference in RFS (p = 0.042) but not in OS (p = 0.713) or MFS (p = 0.845). CONCLUSIONS: Our data suggest more local recurrence after RFA in proven cT1 RCC after adjusting for factors related to treatment selection. This difference does not clearly translate to a greater risk for metastatic progression or, importantly, overall survival. This analysis supports that PN is the gold standard in healthy surgical candidates, but RFA is a reasonable option in those who are of greater surgical risk. 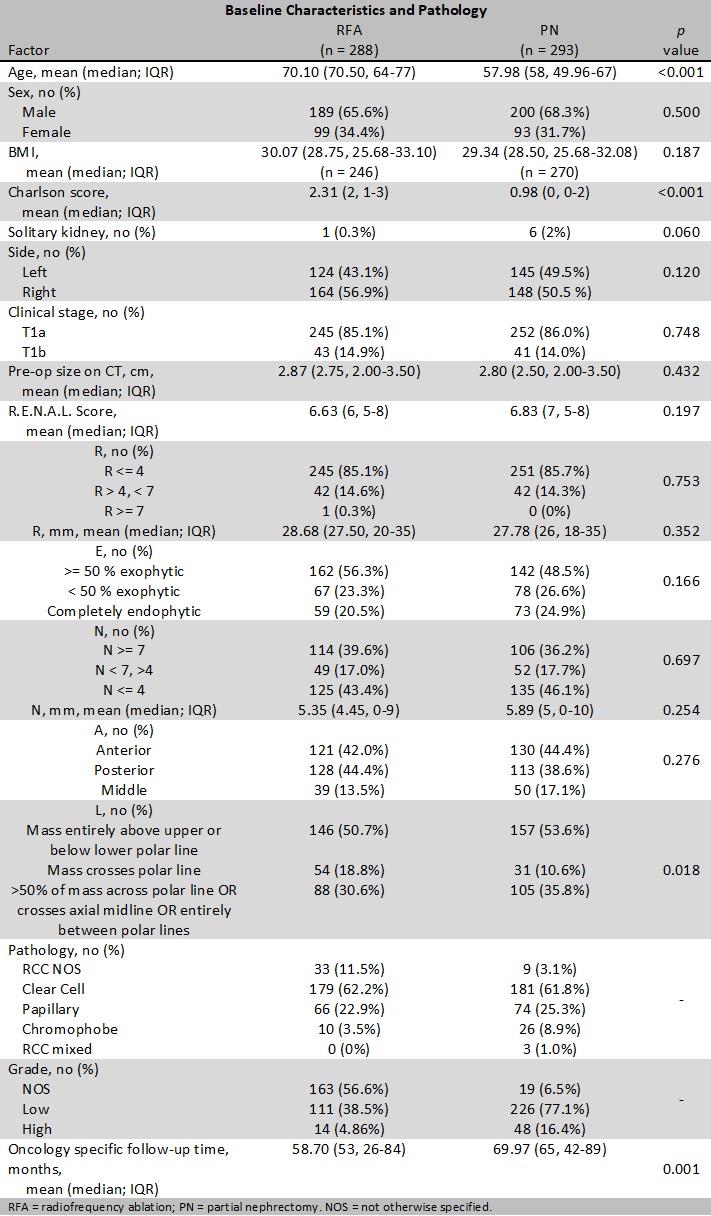
Back to 2018 Program
