Back to 2017 Program
Comparative Effectiveness of Neoadjuvant Chemotherapy vs. Surgery Alone for Upper Tract Urothelial Carcinoma
Kristian D. Stensland, MD, Brendan M. Browne, MD, Marc D. Calabrese, MD, Matthew J. Moynihan, MD MPH, Jared P. Schober, MD, David Canes, MD.
Lahey Hospital and Medical Center, Burlington, MA, USA.
BACKGROUND
Upper tract urothelial carcinoma (UTUC) is an understudied disease with limited large-scale studies providing evidence for treatments. Through analogy to bladder cancer, neoadjuvant chemotherapy (NAC) has been purported to have a potential survival benefit for patients with UTUC. Few studies and no randomized trials explore this issue. We present a case matched comparative effectiveness analysis of NAC compared to surgery alone for patients with UTUC undergoing nephroureterectomy.
METHODS
The National Cancer Database was queried for patients with transitional cell carcinoma of the ureter or renal pelvis, clinical TanyN0M0, without receipt of radiation or adjuvant chemotherapy. NAC patients were propensity score matched 1:5 with surgery alone patients using age, sex, clinical T stage, Charlson comorbidity score, and tumor site; an acceptable covariate balance between groups was assured. Overall survival (OS) was assessed using Kaplan-Meier and multivariate Cox-regression methods were applied to test predictors of OS. A subanalysis additionally matched for pathologic stage.
RESULTS
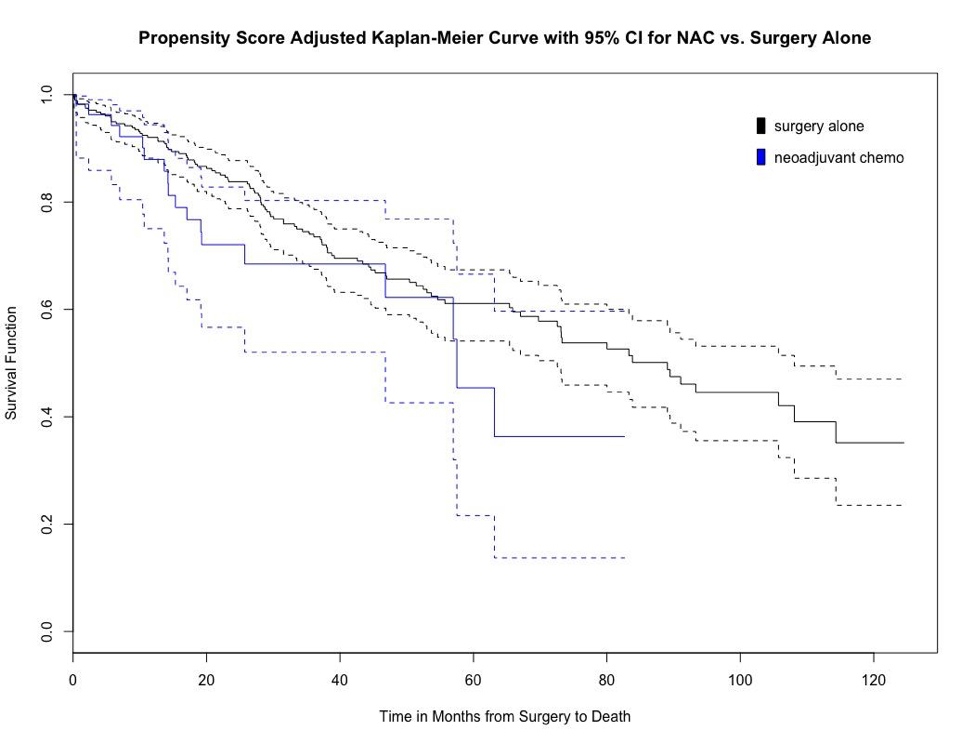
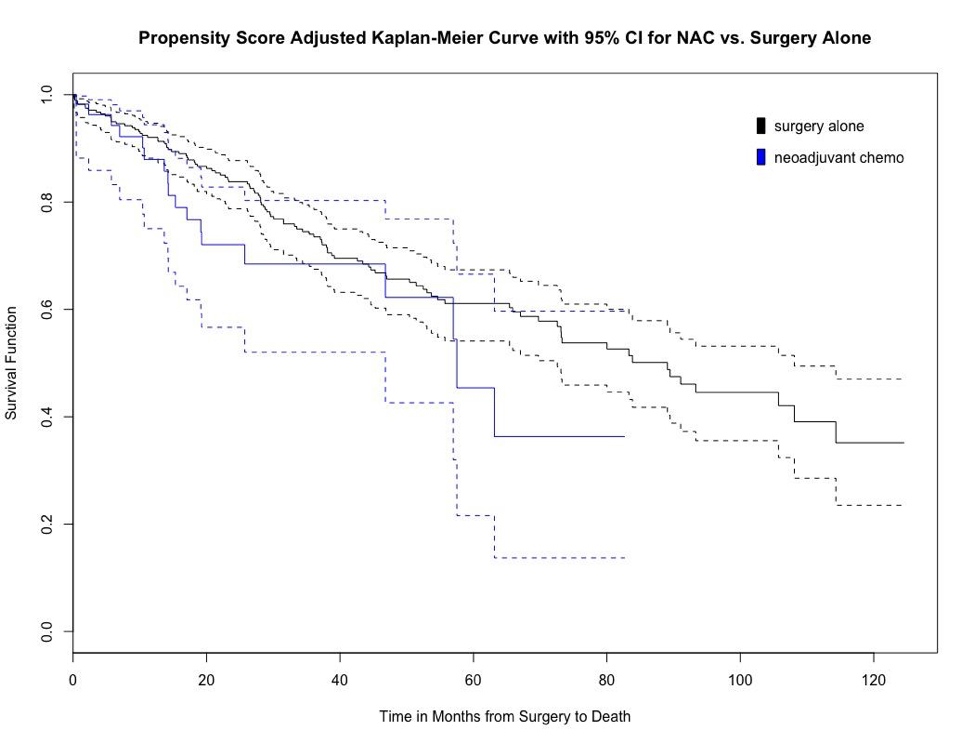
Of 48,845 cases of upper tract cancer, 13,973 cases met inclusion criteria. On Cox regression of the entire included cohort, NAC, age, male gender, ureteral site and advanced T stage were associated with lower OS (p=0.017). The matched sample comprised 112 NAC and 552 surgery alone cases; OS with NAC was lower compared to surgery alone at 5 years but did not reach statistical significance (42.0% vs 53.3% p=0.08) (Figure 1). On subanalysis, a cohort matched for similar variables with the addition of pathologic stage similarly found no difference in OS.
CONCLUSIONS
In this large hospital-based cohort analysis, NAC did not have show a statistically significant difference in OS compared to a case-matched surgery-alone group. While NAC may have no true OS benefit, these results may be affected by unmeasured covariates, as patients thought to have clinically more advanced disease may be selected for NAC, but there is little evidence available for comparison. Notably we could not determine if NAC improves cancer specific survival, as CSS is not recorded in the NCDB. Further study is required to clarify the possible benefits or harms of NAC in this rare disease.
Back to 2017 Program
|
|
|
|