Back to 2017 Program
The use of prostate-specific antigen velocity as a screening tool for pre-biopsy detection of prostate cancer and differentiation of high-grade disease in African American men
Zachary S. Feuer, BS1, Daniel A. Segal, BS1, Clara Oromendia, MS2, Frank A. Myers, Jr., MD3, Samuel Gold, BS1, Jeffrey P. Weiss, MD3, Brian K. McNeil, MD3, Llewellyn M. Hyacinthe, MD3, Andrew G. Winer, MD4.
1SUNY Downstate College of Medicine, Brooklyn, NY, USA, 2Weill Cornell Medicine, Division of Biostatistics and Epidemiology, New York, NY, USA, 3SUNY Downstate Medical Center, Department of Urology, Brooklyn, NY, USA, 4Kings County Hospital Center, Department of Urology, Brooklyn, NY, USA.
Background: The use of a singular prostate-specific antigen (PSA) value as a screening tool for prostate cancer (PCa) in African American men remains controversial. Meanwhile, African American men are at a higher risk for the development of PCa as compared to Caucasians. PSA velocity (PSAV) has been proposed as an alternative screening method, and has demonstrated statistical significance as a predictive model in African Americans, however, sample sizes have been limited. Here, we assess the use of pre-biopsy PSAV, to be used in conjunction with the current standard practice, for the detection of the presence of PCa in one African American population.
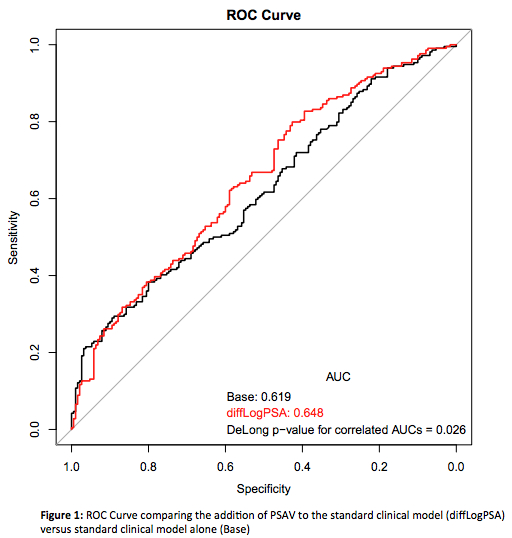
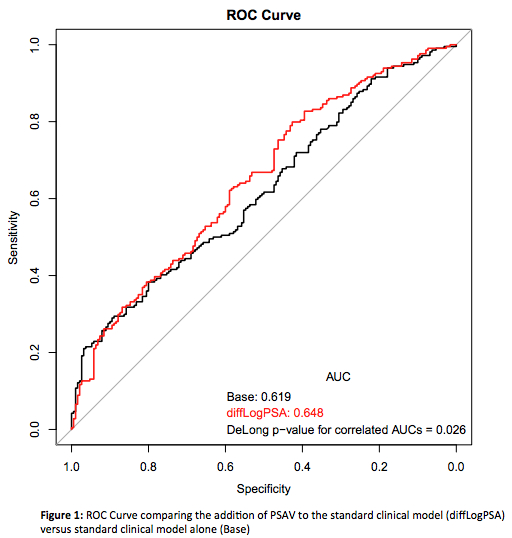
Methods: Demographic data including age, ethnicity, pre-biopsy PSA dates and values, and pathology results were collected from 578 men who underwent prostate biopsy at one institution between 2010-2014. Patients in this cohort were biopsied on the basis of suprathreshold PSA and/or abnormal DRE finding. Exclusion criteria included non-African American patients and patients with any pre-biopsy PSA value greater than 50 ng/mL. PSAV was calculated as the annualized difference in log PSA using the last two PSA values before biopsy. Logistic regression of the odds of having a positive biopsy was used to examine the addition of PSAV to the standard clinical model (age at biopsy, DRE history, and log PSA). Hazard ratio of PSAV was used to examine an association between PSAV and biopsy results, and ROC curves were developed to compare the impact of discrimination using area under the curve (AUC). These methods were repeated for patients with high-grade prostate cancer (HGPC) detection, defined as Gleason 8 or higher.
Results: PSAV improved the prediction of biopsy-proven prostate cancer (AUC 0.65 vs. 0.62, p=0.026) in this African American population when combined with singular PSA values, age and DRE, as shown in Figure 1. PSAV reported as annualized difference in log PSA was 0.17 vs 0.31 (p=0.002) in the biopsy negative and biopsy positive cohorts, respectively. An additional unit increase in PSAV was associated with an 18% increase in the odds of the biopsy being positive for prostate cancer (multivariable p=0.02). The HGPC model yielded similar results with hazard ratios of 1.16 for increasing PSAV (multivariable p=0.05).
Conclusion: PSAV is a significant predictor of the presence of PCa, as well as HGPC, in African American men. In this population, clinicians should consider PSAV, in conjunction with the use of singular PSA values and DRE, when counseling patients regarding prostate cancer risk and the relevance of undergoing prostate biopsy. Future studies should aim to further stratify these results on the basis of Gleason score to establish specific guidelines.
Back to 2017 Program
|
|
|
|
|