Back to 2017 Program
The Association Between Mortality and Distance to Treatment Facility in Patients with Muscle Invasive Bladder Cancer
Emily C. Serrell, MS1, Stephen T. Ryan, MD2, Patrick Karabon, MS3, Gregory J. Mills, BA1, Moritz H. Hansen, MD1, Matthew Hayn, MD2, Mani Menon, MD3, Quoc Dien-Trinh, MD4, Firas Abdollah, MD3, Jesse D. Sammon, DO1.
1Center for Outcomes Research and Evaluation, Portland, ME, USA, 2Maine Medical Center, Portland, ME, USA, 3Henry Ford Health System, Detroit, MI, USA, 4Brigham and Women's Hospital, Boston, MA, USA.
BACKGROUND: Regionalization of bladder cancer treatment is suggested to improve quality of care. As an unintended consequence, patients are faced with increased distance between home and treatment facility, with unknown implications on outcomes. We characterize the effect of distance on overall mortality in patients with muscle invasive bladder cancer (MIBC) and those who undergo radical cystectomy (RC).
METHODS: We used the National Cancer Database (2004-2012) to identify patients with clinically localized, muscle invasive bladder cancer (cT2a-T4,N0M0); sub-group analysis of RC patients was performed. Multivariate Cox Proportional Hazard and multinomial logistic regression analyses were performed to evaluate the relationship between mortality and distance from treatment facility. Subgroup analysis of treatment type and clinical stage at diagnosis were performed. Models were adjusted for demographic, clinical, hospital, and geographic factors.
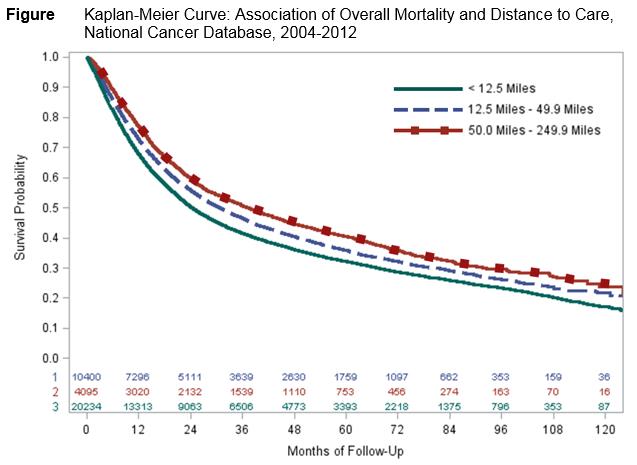
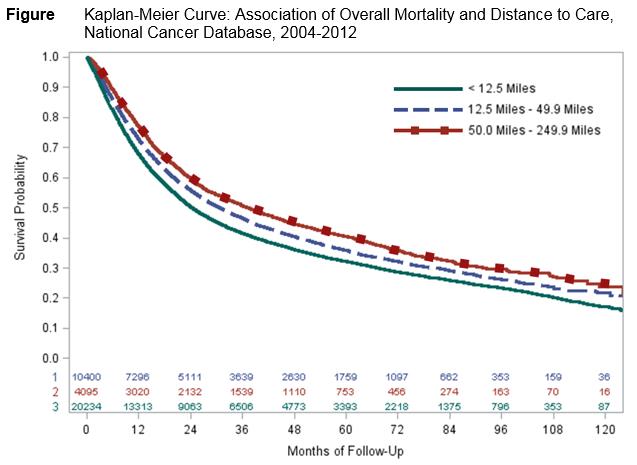
RESULTS: For 34,729 patients with MIBC, traveling farther for treatment was associated with lower probability of mortality (referent <12.5 miles: 12.5-49.9 miles hazard ratio (HR)=0.96, 95% confidence interval (CI) 0.92-0.99; 50-250 miles HR=0.91, 95% CI 0.86-0.96; Figure). This was significant for patients with cT2 disease, as well as for those who were treated at academic centers (all p<0.05). Patient factors associated with receiving care close to home-older age, non-Hispanic black race, female gender, more comorbidities, Medicaid or no insurance, lower educational attainment - were also associated with increased probability of overall mortality (all p<0.05).
For the 11,059 patients who underwent radical cystectomy, the distance-mortality trend did not reach significance (referent <12.5 miles: 12.5-49.9 miles HR=0.96, 95% CI 0.90-1.03; 50-250 miles HR=0.94, 95% CI 0.86-1.03). However, longer distance to care was associated with surgery at a high-volume institution and receipt of neoadjuvant chemotherapy (all p<0.001). There was no significant association between distance and stage at diagnosis of MIBC in either the full or subgroup samples.
CONCLUSIONS: Although regionalization has resulted in increased distance to care, this study suggests that there is no direct negative impact on survival. Patients who travel for care of muscle invasive bladder cancer have a lower risk of overall mortality compared to those who live closer to their treatment facility, particularly if traveling for treatment at academic facilities. In patients who underwent RC, the association between distance and mortality was equivocal. However, traveling farther was associated with higher receipt of neoadjuvant chemotherapy and treatment at a higher volume facility. The reasons for this greater travel distance-decreased mortality finding are difficult to ascertain, though we believe it may be related to a complex association between regionalization of MIBC and RC care and healthcare seeking behaviors. Future research should evaluate patient preferences regarding distance to treatment, as well as the effect of distance and access to care in vulnerable sociodemographic populations.
Back to 2017 Program
|
|
|
|
|