Back to 2017 Program
Diagnosis and Management of Urachal Remnants in a Tertiary Care Center
Marc D. Calabrese, MD1, Kristian D. Stensland, MD1, Jared Schober, MD1, Usama Siddique, BS2, Ariel K. Fredrick, MD1, Jennifer Broder, MD1, Alireza Moinzadeh, MD1.
1Lahey Hospital and Medical Center, Burlington, MA, USA, 2Tufts University School of Medicine, Boston, MA, USA.
INTRODUCTION
Urachal remnants are classically taught as potential causes of clinical symptoms, such as umbilical drainage, infections, or hematuria; there is also a theoretical risk of transition to urachal adenocarcinoma. To date, the incidence of urachal remnants, patterns of management, and malignant transitions have not been quantified. We queried our institution’s radiology database to establish and investigate a cohort of patients with an identified urachal remnant.
METHODS
Under institutional IRB protocol, all radiology reports from 2012-2015 at a single tertiary care center were queried for the term “urach*”, and radiographic, clinical, and surgical/pathologic information on identified patients was then extracted by hand from the EMR. Symptomatic urachal remnants were defined by the symptoms given in the reason for the radiology scan. Patients with an already identified urachal remnant prior to the scan were excluded. Descriptive statistics, chi-squared and t-tests for comparisons were used as appropriate and statistical analysis was performed in R.
RESULTS
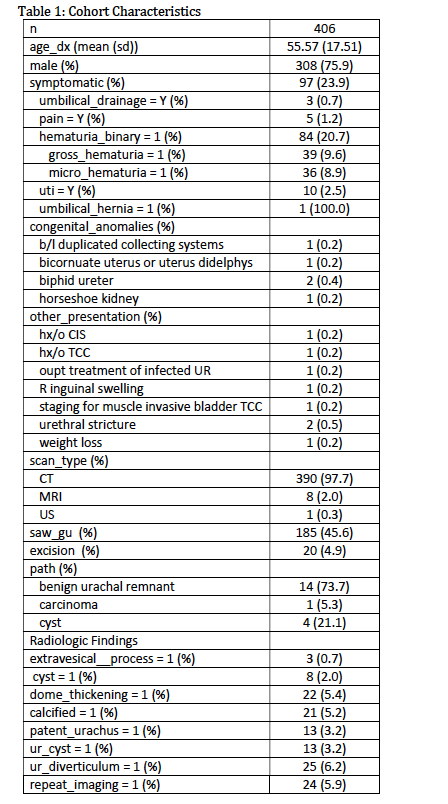
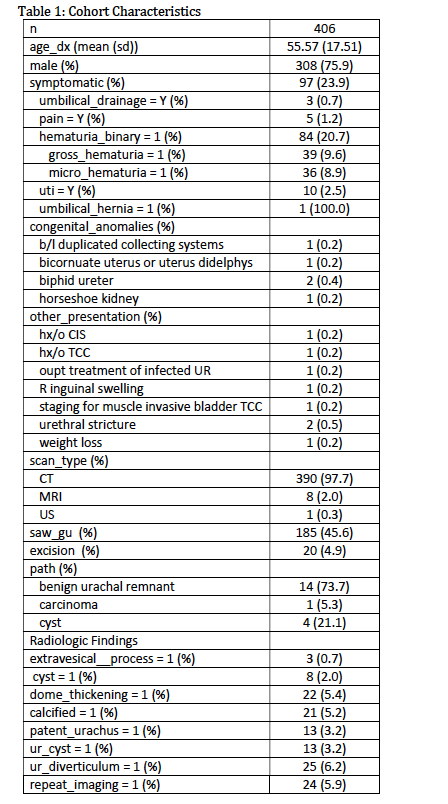
A total of 406 patients had urachal abnormalities on radiology scans. Characteristics of the patients, along with radiologic and clinical findings and surgical management, are in Table 1. Of the 406 patients identified, 97 (23.9%) had symptoms related to a urachal remnant cited as a reason for the scan, the most common reason being hematuria (84 patients, 20.7% of total cohort). A total of 185 patients (45.6%) were referred to urology, and 20 (4.9%) had excision of the urachal remnant. Path data were available for 19 cases; of these, only one was positive for urachal adenocarcinoma.
CONCLUSION
Urachal remnants are a rare entity, with a majority incidentally discovered. Less than half of identified cases are referred to urology, and excision is uncommon. Malignant transformation is rare. In the future, exact classification of urachal remnants and guidelines for referral to urology, as well as further clinical and pathologic follow-up, are needed to refine recommendations for treatment of this rare condition.
Back to 2017 Program
|
|
|
|