Back to 2017 Program
A study of resident sleep patterns in relation to volume and category of overnight pages in a home call system
Adam Ludvigson, M.D., Gregory Mills, B.A., Stephen T. Ryan, M.D., Graham VerLee, M.D., Moritz Hansen, M.D..
Maine Medical Center, Portland, ME, USA.
BACKGROUND: Mitigating resident fatigue is central to the design and implementation of residency programs, especially when using a home call system. Existing studies of resident sleep habits and fatigue are mostly limited to in-house call and rely on self-reporting. We quantified time spent asleep for residents in a home call system, and examined how the volume and type of pages received affected sleep.
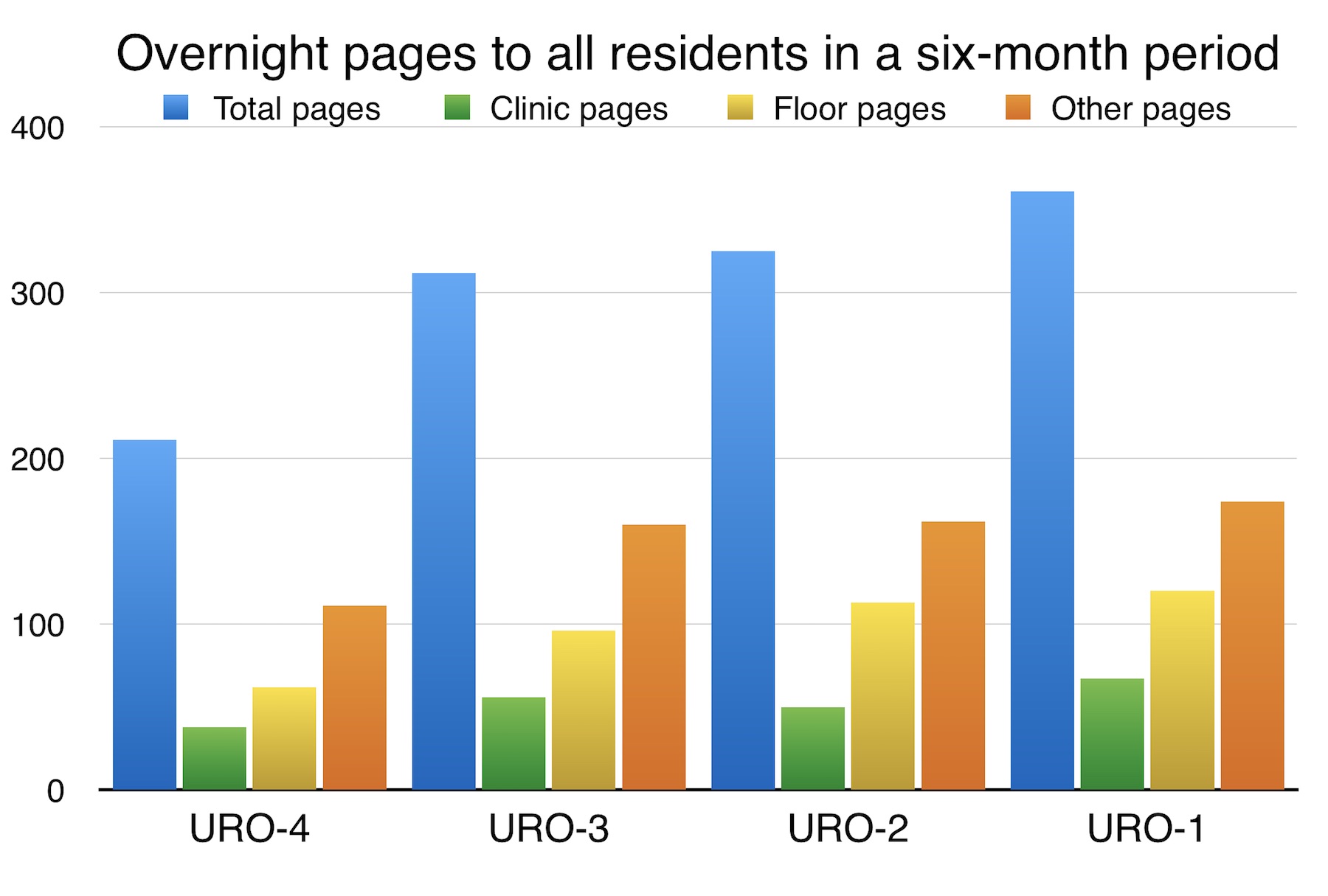
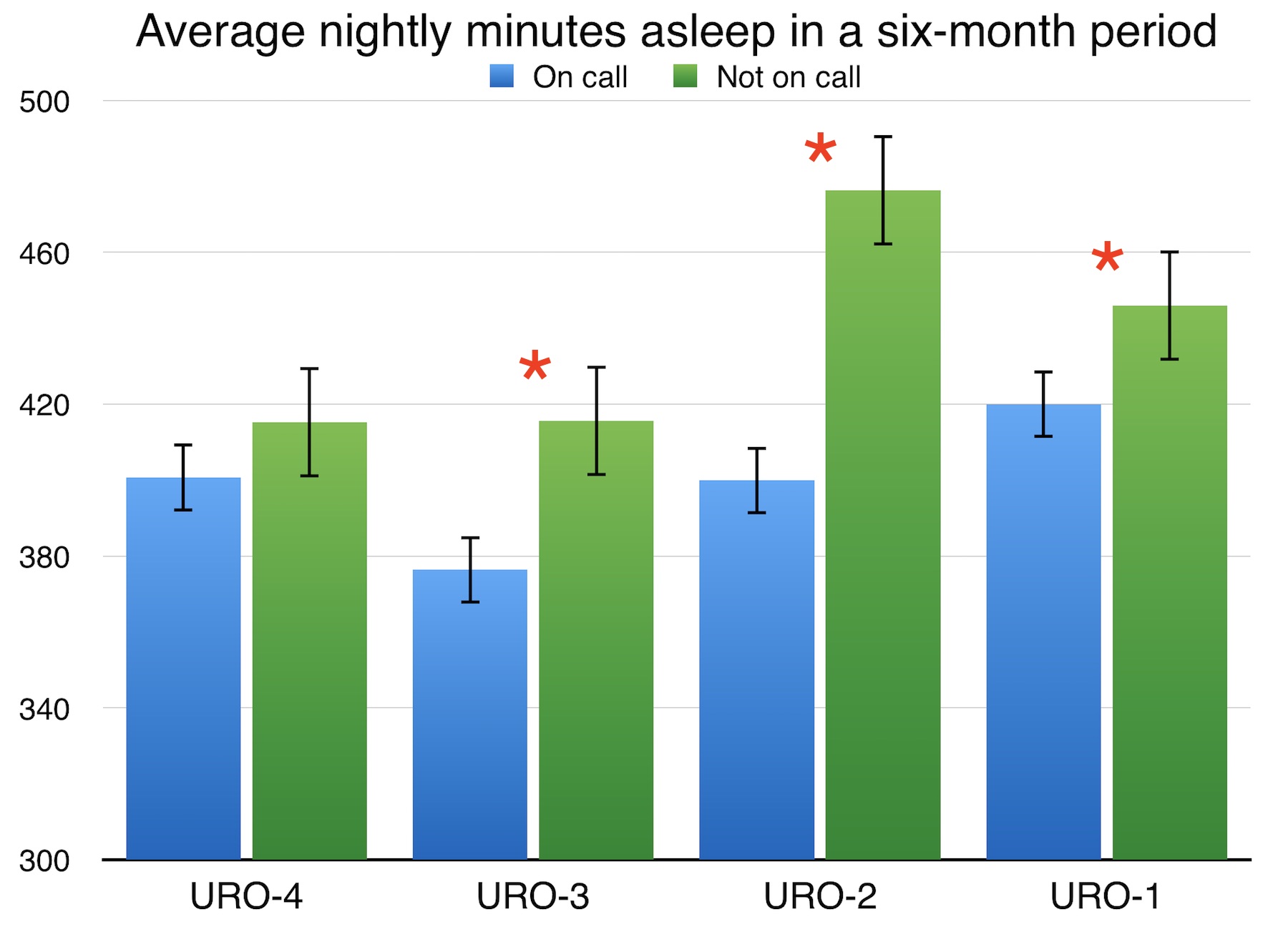
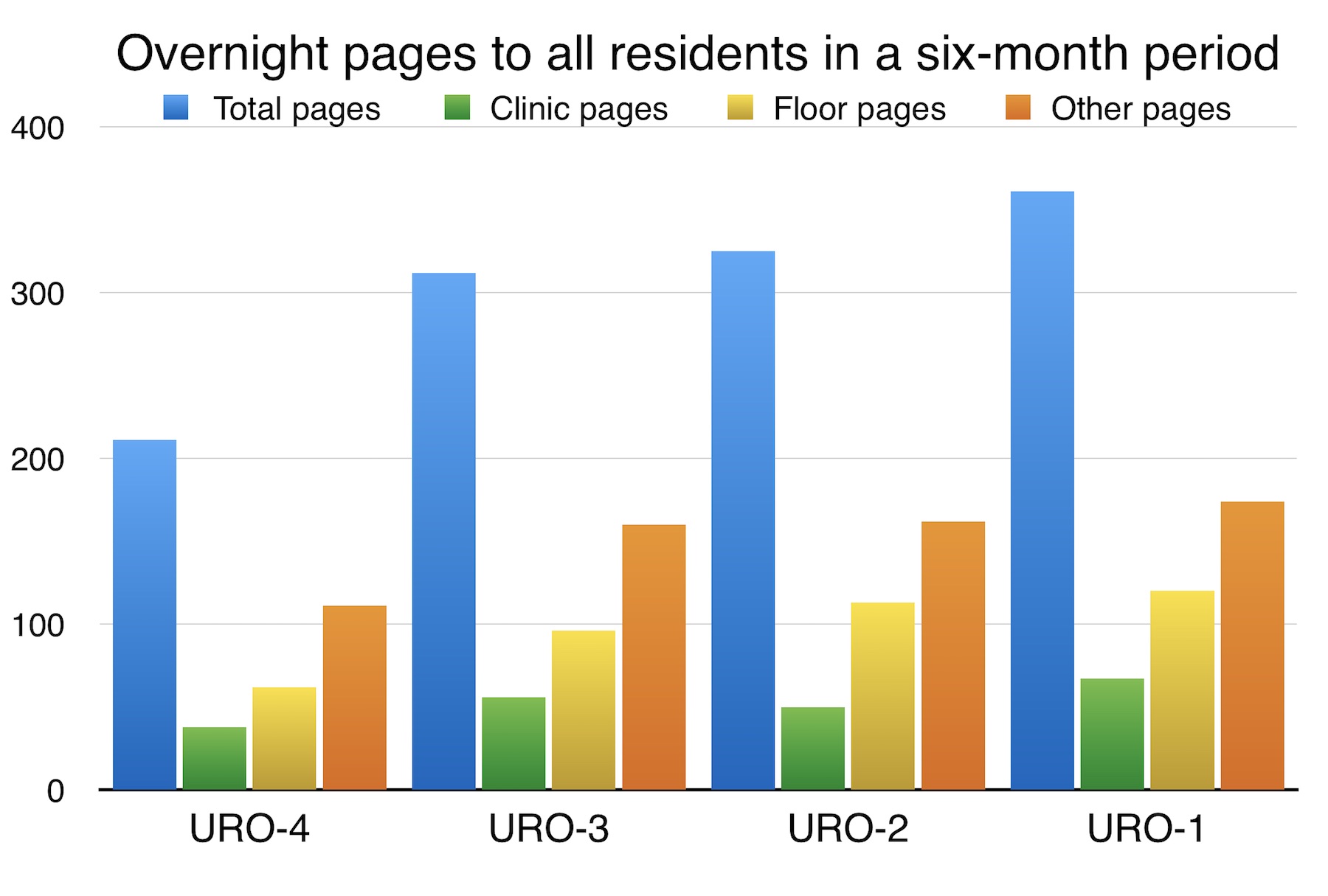
METHODS: Urology residents in a single-institution residency were provided with a FitBit Charge HR device to collect objective sleep data over a six-month period. Each page received during this period after 16:00 and before 08:00 was counted and categorized as either “clinic” (outpatient calls from the after-hours answering service), “floor” (calls from the inpatient urology ward), or “other” (calls regarding off-floor consults). Data analysis was carried out using IBM® SPSS® Statistics 23 and Numbers.
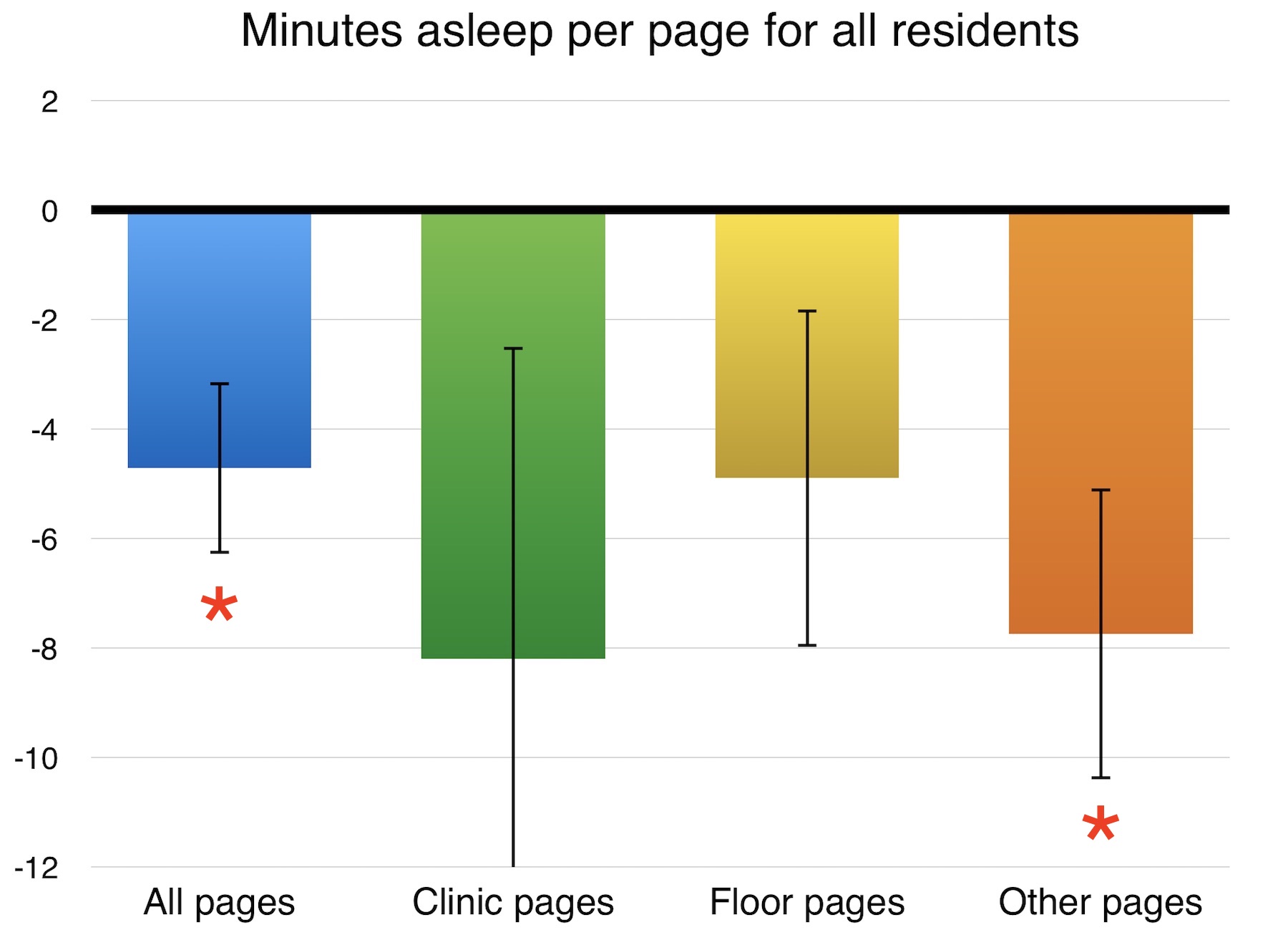
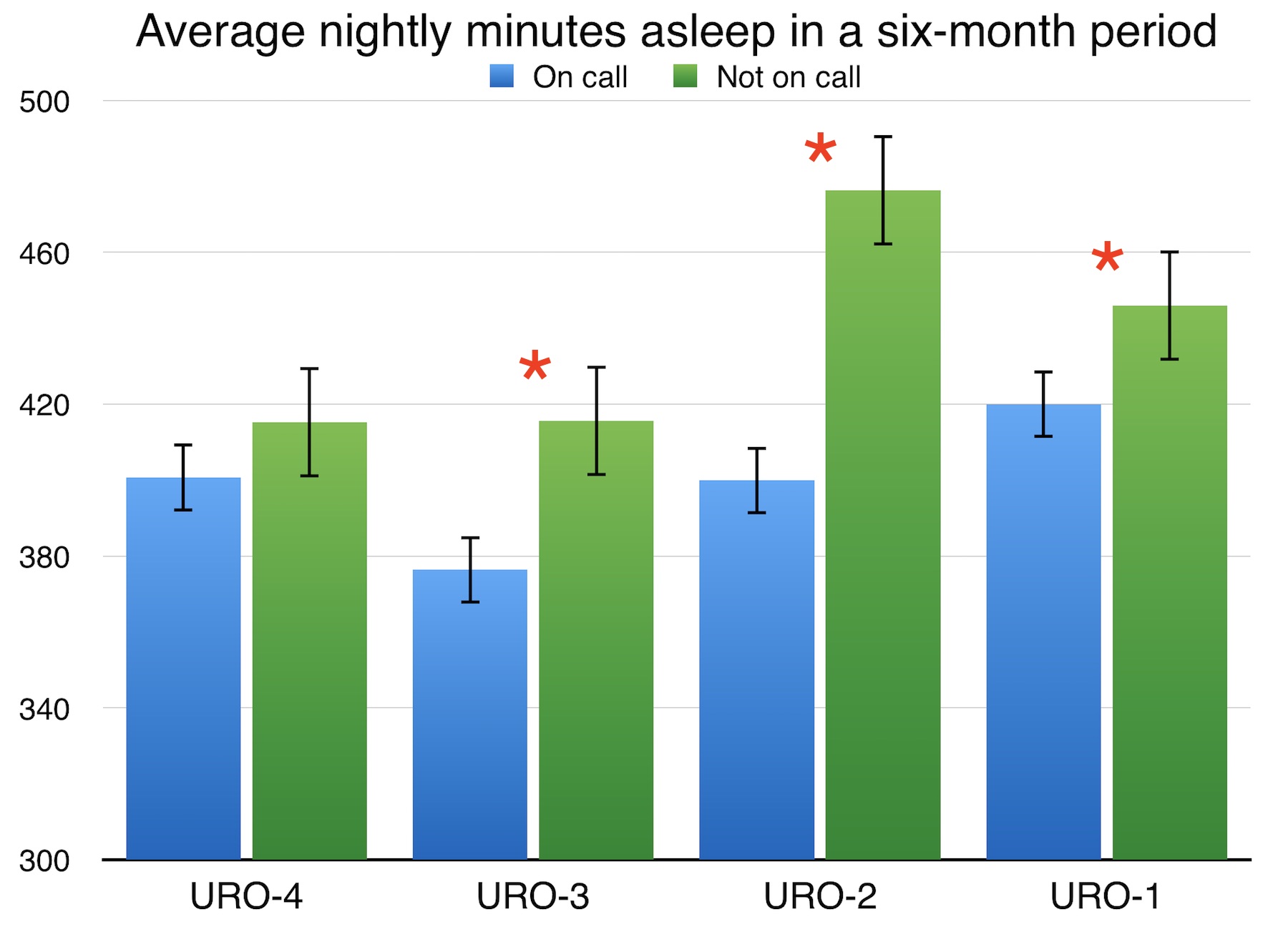
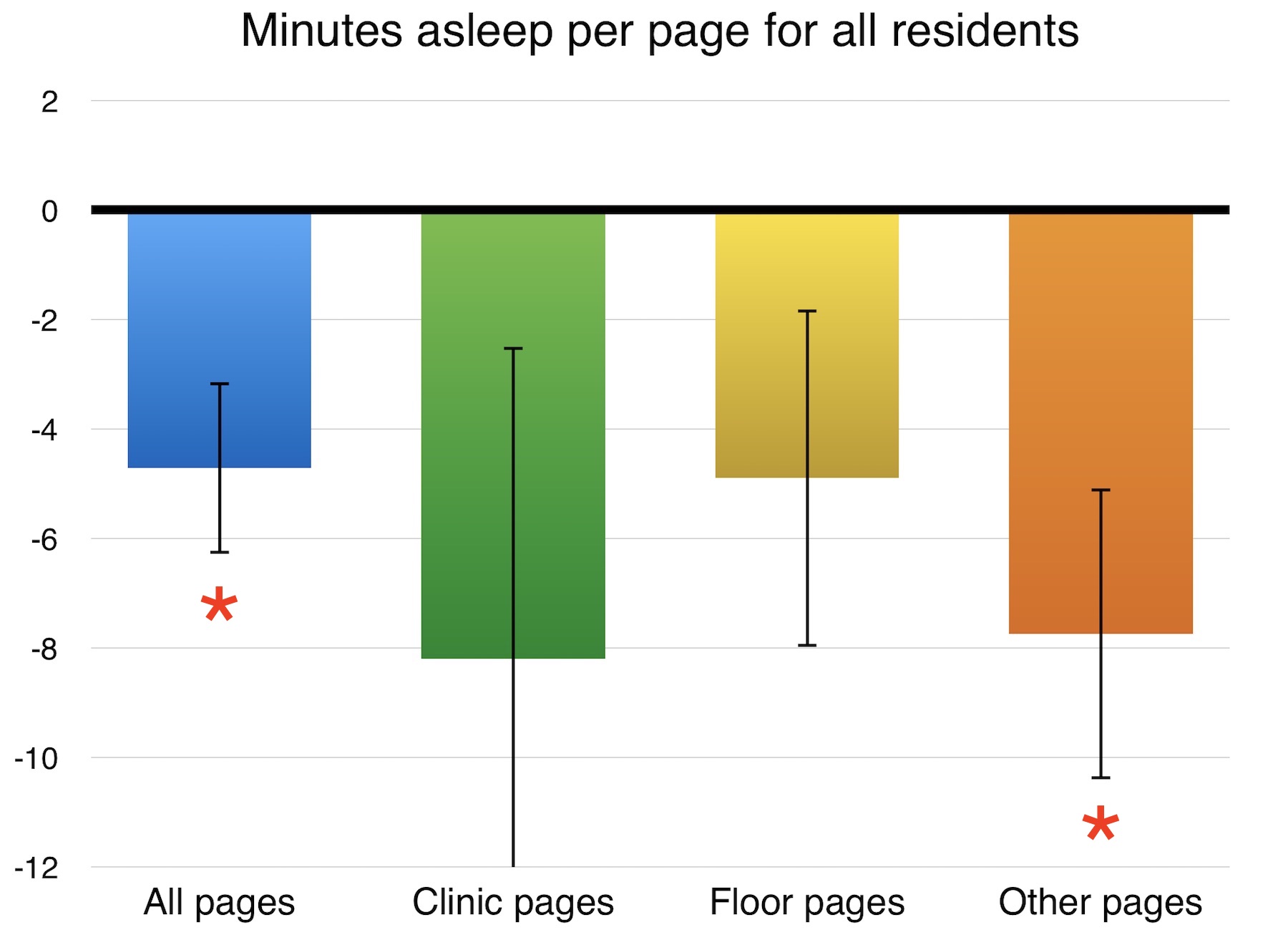
RESULTS: Residents received a total of 1068 overnight pages while on call. The junior (URO-1) resident received 321 (avg. 7.0/night) pages, followed by 288 (avg. 6.0/night), 265 (avg. 6.3/night), and 194 (avg. 5.0/night) for the next three most senior residents (URO-2, -3, and -4), respectively. On average, residents slept 400 minutes while on call, compared to 436 minutes while not on call (p<0.05). Each page was associated with 4.71 fewer minutes asleep per page for all residents (r=-0.24, n=145, p<0.05). Pages in the “other” category were associated with 7.74 fewer minutes asleep per page for all residents (r=-0.24, n=145, p<0.05). On individual analysis, each page to the junior resident from all categories was associated with 4.23 fewer minutes asleep (r=-0.33, n=44, p<0.05), and each page from the “floor” category was associated with 9.02 fewer minutes asleep (r=-0.35, n=44, p<0.05).
CONCLUSIONS: Call volume decreased steadily with increasing resident seniority, an interesting finding considering that call nights were evenly distributed. This may imply that experience allows senior residents to anticipate problems in order to prevent calls before they happen. Residents slept less on call in general. Time asleep was reduced with increasing page volume, most significantly when pages were from the “other” category, suggesting more time is needed to address pages regarding patients the resident is unfamiliar with. Calls from the floor were more detrimental for the junior resident only, indicating that experience is a factor for efficient overnight call management. Overall, these findings are the first to objectively measure sleep quality in relation to call volume and type within a home call system, and show that efficient call management is a learned skill that improves throughout residency.
Back to 2017 Program
|
|
|
|