Back to 2017 Program
Prostate Cancer Screening in Early Medicaid Expansion States
Emily C. Serrell, MS1, Jesse D. Sammon, DO1, Patrick Karabon, MS2, Gregory J. Mills, BA1, Mani Menon, MD2, Firas Abdollah, MD2, Quoc Dien-Trinh, MD3.
1Center for Outcomes Research and Evaluation, Portland, ME, USA, 2Henry Ford Health System, Detroit, MI, USA, 3Brigham and Women's Hospital, Boston, MA, USA.
BACKGROUND: The Affordable Care Act of 2010 included a provision to expand Medicaid for low-income individuals, and six states jurisdictions (CA, CT, DC, MN, NJ, WA) elected to expand Medicaid early, before the 2014 implementation. This study aimed to assess whether Medicaid early expansion and the accompanying improved healthcare coverage was associated with increased preventive care utilization, including prostate specific antigen (PSA)-based prostate cancer screening.
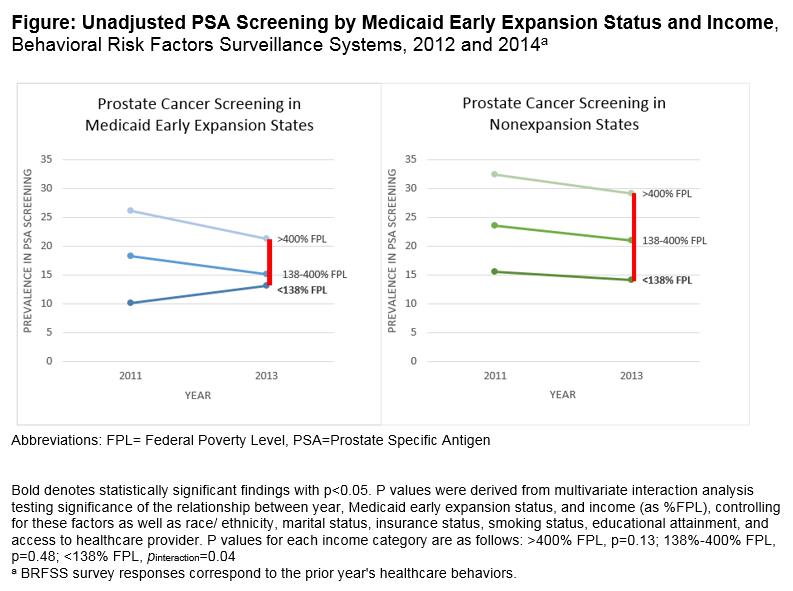
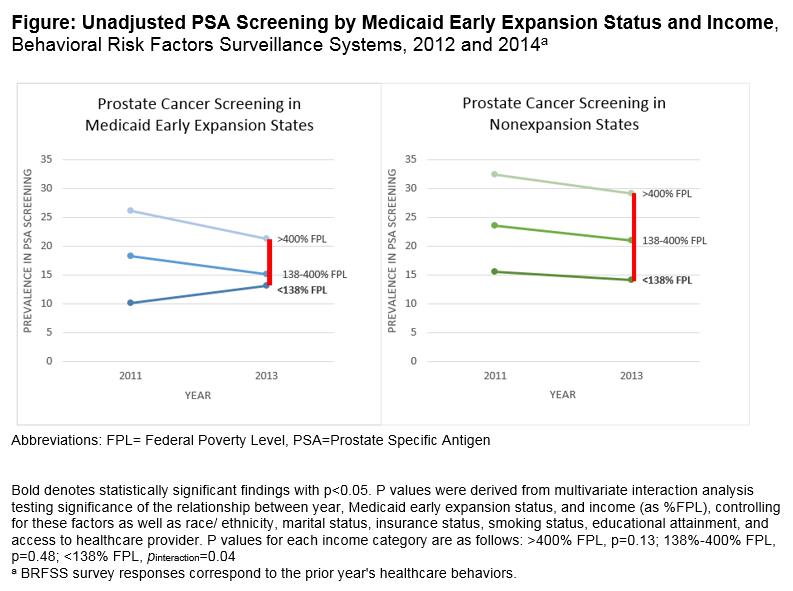
METHODS: Data from the 2012 and 2014 Behavioral Risk Factor Surveillance System were used to determine prostate cancer screening rates in men who were aged 40-64, asymptomatic, without prostate cancer, and self-reported a PSA testing in the past 12 months. Sociodemographic and access to care variables were extracted, and income categories were stratified by relationship to Medicaid eligibility and federal poverty level (<138%, 138-400%, >400%). Unadjusted weighted PSA prevalence was estimated. After adjustment, multivariable logistic regression models evaluated the odds of PSA screening in early expansion versus non-expansion states. Interaction analyses were performed to determine effect of Medicaid expansion on screening, and sensitivity analysis excluding health access covariates (insurance, access to healthcare provider) was performed.
RESULTS:Among 158,103 survey respondents, individuals in non-expansion states had the highest rates of screening. Nationally, screening decreased between 2011 and 2013 (Odds Ratio=0.87, 95% Confidence Interval 0.83-0.91) regardless of expansion status. In early expansion states only, there was a 3% absolute increase in screening among men <138% FPL that was associated with expansion status (Pinteraction=0.04; Figure). Sensitivity analysis excluding health access variables demonstrated no significant changes. Increased screening in early expansion states was also seen in men who were aged 55-59 (+1.8%), non-Hispanic black (+1.7%) and Hispanic (+1.7%) races, previously married (+1.3%), not high school graduates (+1.7%), and current smokers (+2.1%).
CONCLUSIONS: Between 2011 and 2013 there were national declines in prostate cancer screening that have been well-studied in relation to the US Preventive Services Task Force 2012 recommendation against screening. However, PSA screening increased among low-income residents of Medicaid early expansion states, particularly among Hispanic and non-Hispanic black males. This increase may have been attributable to improved access to preventive services among populations with historic barriers to care, as reflected by the significant narrowing of the gap in PSA screening between high- and low-income populations in Medicaid early expansion states. Future research is needed to examine whether Medicaid expansion is associated with changes in additional cancer metrics—e.g. time to diagnosis, time to treatment, morbidity and mortality outcomes— particularly given the uncertain benefit of PSA screening in the broad population.
Back to 2017 Program
|
|
|
|
|