Back to 2017 Program
How much is just right? An evaluation of post-operative opioid prescribing for urologic procedures at a single institution
Kathleen M. Olson, BS, Theodore Cisu, BS, Peter Holoch, MD, Mayo H. Fujii, MD, Thomas P. Ahern, PhD, MPH, Charles D. Maclean, MD.
University of Vermont, Burlington, VT, USA.
BACKGROUND: Opioids prescribed at hospital discharge after a surgical procedure are a potential source of diversion and misuse. Given the increase in opioid abuse over the past decade, it is critical that surgical specialties, including urology, examine opioid prescribing practices to prevent over-prescribing. The optimal quantity of opioid medication prescribed at hospital discharge after urologic surgery has not been well defined. In this study, we summarize opioid prescription and use patterns among patients undergoing urologic procedures, including vasectomy, common endoscopic procedures, and robotic-assisted laparoscopic prostatectomy (RALP).
METHODS:We recruited patients who underwent vasectomy, endoscopy, or RALP at a single institution between October 2016 and February 2017. The endoscopy group included patients who underwent cystoscopy with cystolithopaxy, ureteroscopy, lithotripsy, or stent placement. Reasons for exclusion included age under 18, underlying malignancy, bilateral procedure (except vasectomy), recent procedure on the same ureter within the past month, additional procedures such as ureteral biopsy, procedural complication, inability to communicate independently over telephone, and refusal to participate. Patients were called 5-7 days post-discharge and given a 26-item telephone survey inquiring about amount of opioid used, patient-perceived pain control, and discharge instructions. Opioid prescription details were confirmed using the electronic medical record with patient permission.
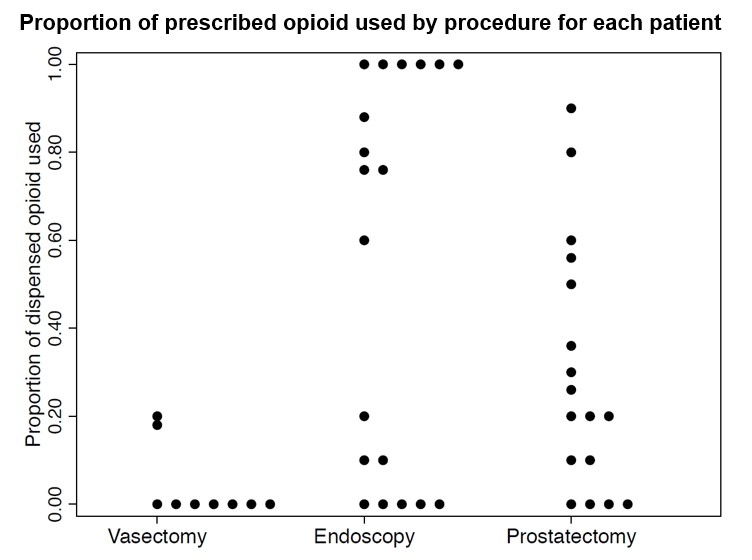
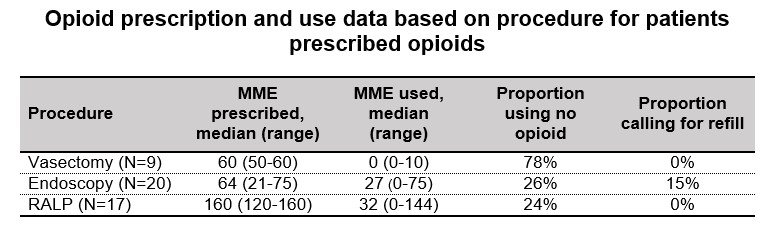
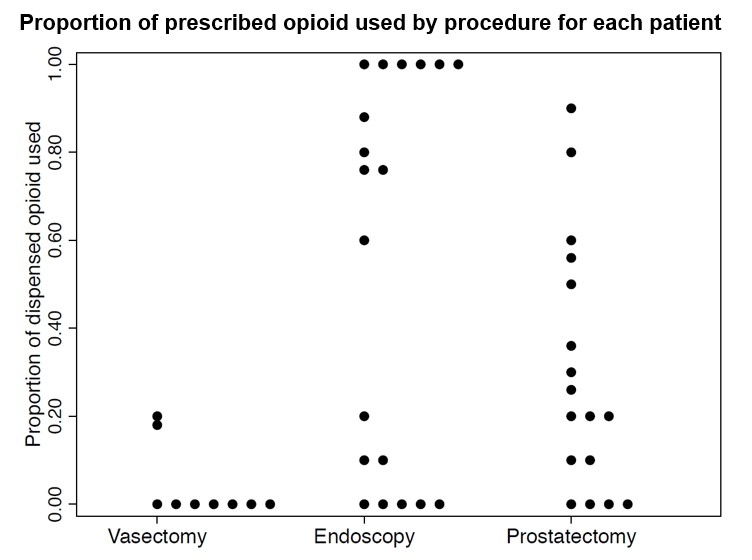
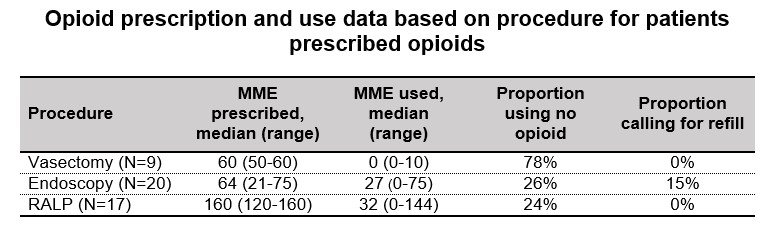
RESULTS: A total of 57 patients (median age=56) underwent either vasectomy (n=10), endoscopy (n=30), or RALP (n=17) and met inclusionary criteria. Of the enrolled patients within each group, 90% of vasectomy, 67% of endoscopy, and 100% of RALP patients received an opioid prescription (total n=49). The most commonly prescribed opioid was hydromorphone (54%), followed by oxycodone (26%) and hydrocodone (20%). The median MME prescribed were: 60 (vasectomy), 64 (endoscopy), and 160 (RALP). Median MME used for vasectomy, endoscopy, and RALP were 0, 27, and 32, respectively (Figure). Among the subset of patients who received an opioid prescription, 78% of vasectomy, 26% of endoscopy, and 24% of RALP patients did not use any of their prescription after discharge (Table and Figure). Only 13% of patients used their entire prescription and 3 patients (6.5%) called for a refill—all of whom were in the endoscopy group. Only 11% of patients prescribed an opioid reported that they had received instructions for safe drug disposal.
CONCLUSIONS: Most patients received opioids post-operatively and used less than half of their prescription. These results suggest that over-prescription of opioids is common after urologic procedures. Unfortunately, few patients reported receiving instructions for safe disposal of unused opioid. Further studies should determine optimal MME dosing by procedure and evaluate risk factors for higher opioid use post-operatively, especially among patients undergoing endoscopic procedures. In addition, efforts should be made to educate patients on safe opioid disposal.
Back to 2017 Program
|
|
|
|
|