Back to 2017 Program
Transgender Sperm Cryopreservation: Trends and Findings in the Past Decade
Kai Li, MD1, Dayron Rodriguez, M.D.1, Joseph S. Gabrielsen, M.D., Ph.D1, Amy Blanchard, B.S.2, Grace Centola, Ph.D2, Cigdem Tanrikut, M.D.1.
1Massachusetts General Hospital, Boston, MA, USA, 2New England Cryogenic Center, Boston, MA, USA.
Background:
Awareness and acceptance of transgenderism has increased in the last two decades. The 2001 World Professional Association for Transgender Health’s Standards of Care advocates discussion of reproductive issues with transgender patients prior to initiation of hormonal therapy. To date, there is limited literature regarding the incidence and semen characteristics of transgender individuals banking sperm. We sought to assess transgender sperm cryopreservation compared to the non-transgender population in the last 10 years. We also compared semen parameters between the two populations. We hypothesized that there would be an increased incidence of transgender sperm cryopreservation over the last 10 years, corresponding to increasing awareness, and no difference in semen parameters between the two groups.
Methods:
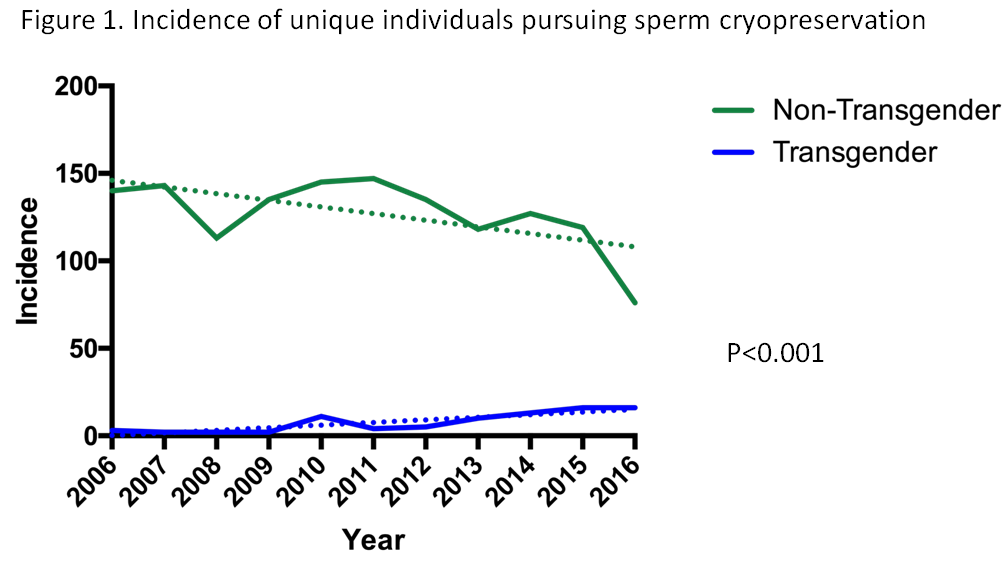
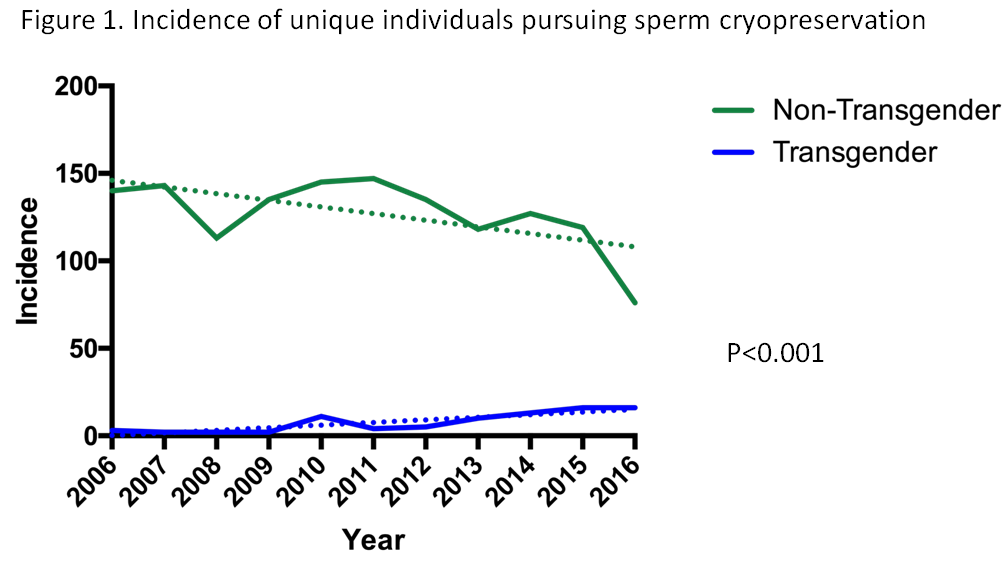
We performed a retrospective analysis of sperm cryopreservation performed at a single center from 2006 through 2016. We analyzed 194 transgender samples and 2327 non-transgender samples for a total of 84 unique transgender bankers and 1398 unique non-transgender bankers. Bankers who preserved multiple samples had the collective semen parameters averaged and the mean used for statistical analysis. Semen samples were analyzed according to WHO 4th and 5th edition guidelines based on year of sample production. Linear regression was used to compare the annual incidence of cryopreservation from 2006-2016 of transgender versus non-transgender. Semen parameters were compared using Student’s T-test.
Results:
The number of transgender individuals pursuing sperm cryopreservation increased relative to non-transgender individuals from 2006 to 2016. The trajectory of the two groups was significantly different (Figure 1, p<0.001). There were no significant differences in ejaculatory volume, total sperm count, percent motility, or total motile sperm between the two groups.
Conclusions:
This is the largest report to date on the incidence of transgender sperm cryopreservation and comparison of semen characteristics. The incidence of sperm cryopreservation by transgender individuals has increased in the last decade, paralleling the increase in awareness and acceptance, and may reflect increased discussion between transgender individuals and medical professionals. As expected, there were no significant differences in semen parameters.
Back to 2017 Program
|
|
|
|