Back to 2017 Program
Regional Variation in Diagnostic Testing for Overactive Bladder in the Female Medicare Population
Annah J. Vollstedt, MD, Rachel Moses, MD, MPH, E. Ann Gormley, MD.
Dartmouth Hitchcock Medical Center, Lebanon, NH, USA.
Title: Regional Variation in Diagnostic Testing for Overactive Bladder in the Female Medicare Population
Introduction:
Overactive bladder (OAB) remains a common urologic ailment with direct healthcare costs now exceeding billions annually.1 The American Urology Association (AUA) released the non-neurogenic OAB guideline in 2012 and amended the treatment section in 2014 in order to guide the diagnosis and management of this costly ailment. Per the guidelines, OAB is a clinical diagnosis requiring only a careful history, physical exam, and urinalysis. Further, additional work-up including post-void residual, urodynamics, cytology, and cystoscopy are not necessary in the otherwise uncomplicated patient.2 The purpose of this study is to determine rates of potentially unnecessary diagnostic testing in patients carrying an OAB diagnosis before and after the OAB guidelines publication.
Methods:
Using the Dartmouth Institute’s Atlas Rate Generator exploring a 100% Medicare claims data sample, we identified females with a diagnosis of OAB by ICD-9 codes within 306 hospital referral regions (HRR). The sample includes patients seen by any provider who makes the diagnosis of OAB. Rates of diagnostic tests within HRR were compared to the national average adjusted by age and race. We excluded those beneficiaries who had a CPT code for a third line treatment of OAB.
Results:
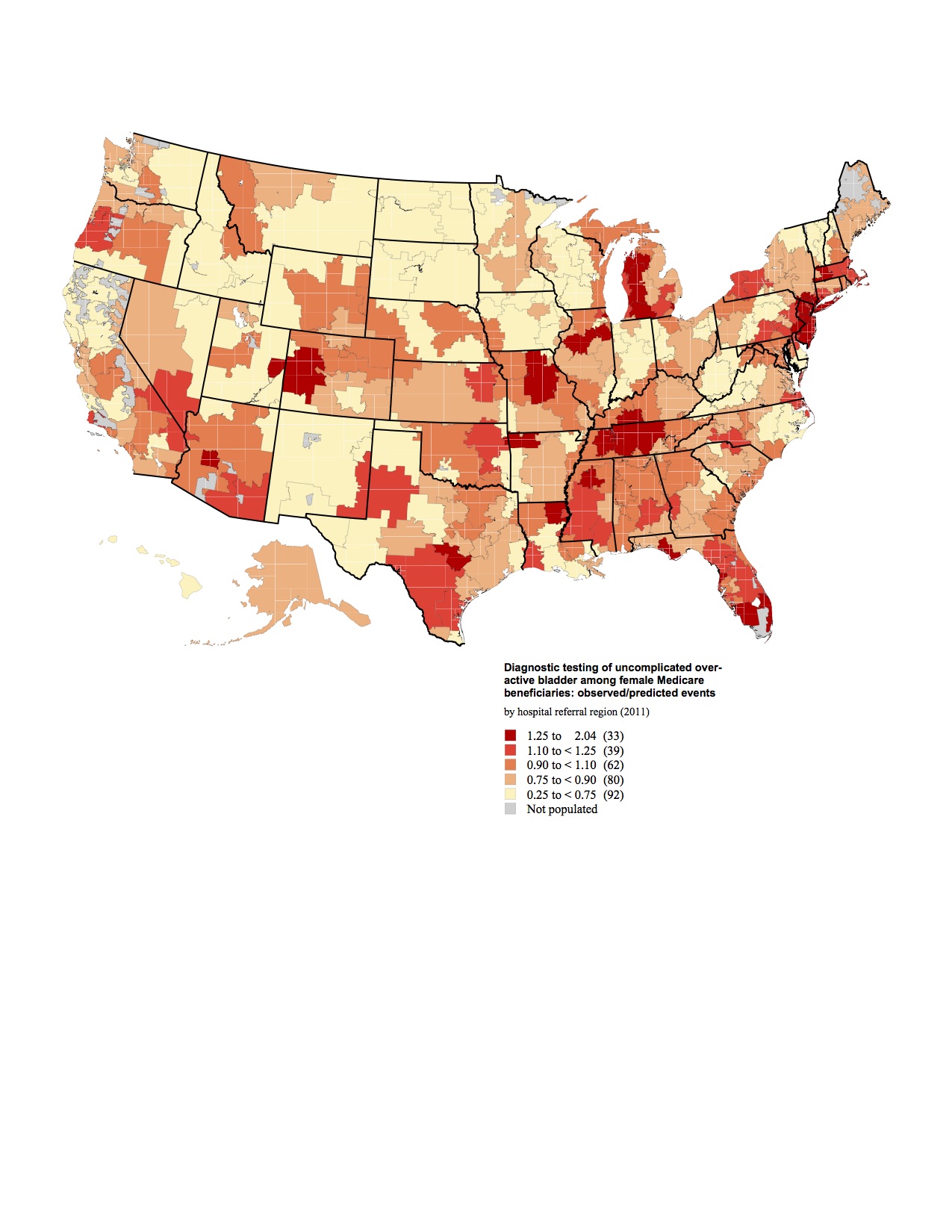
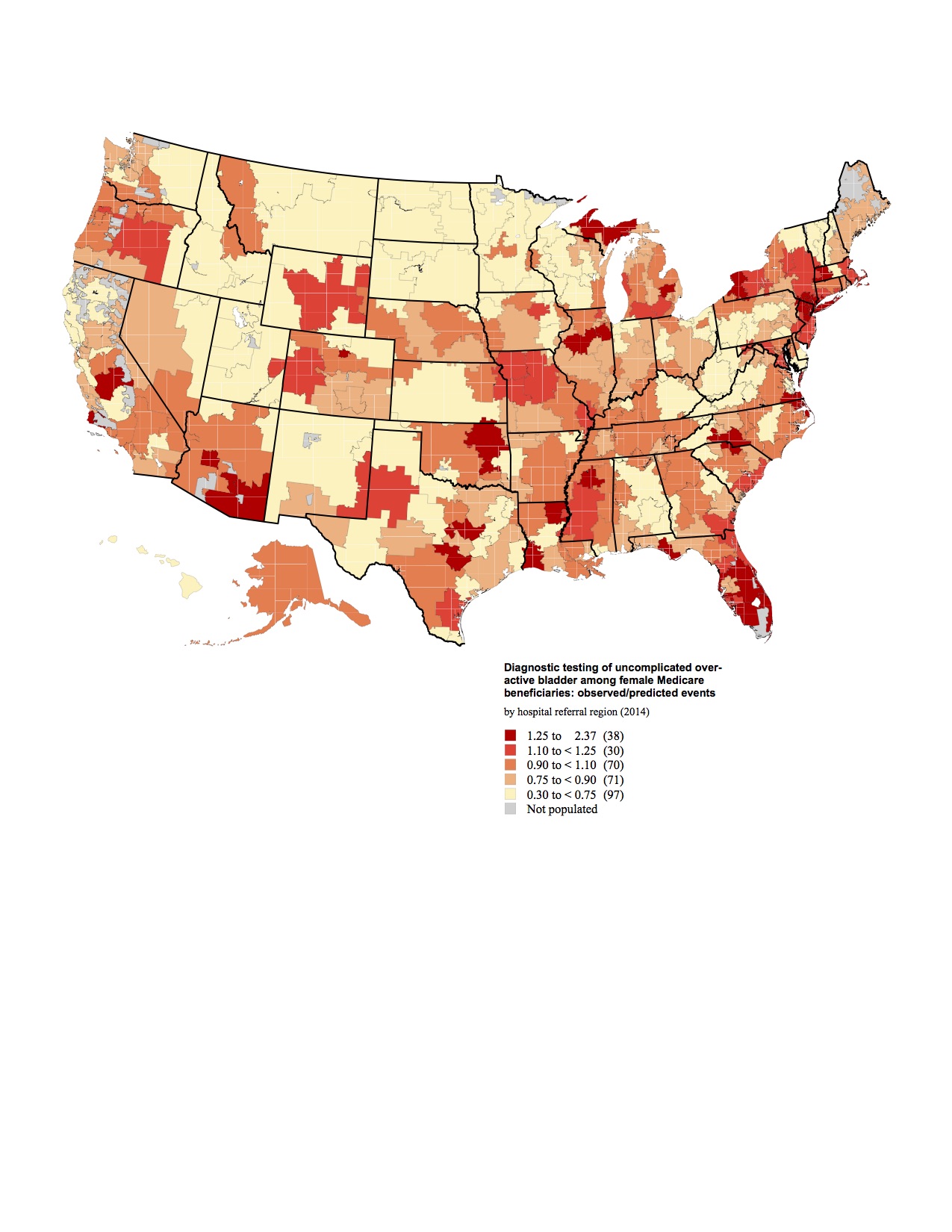
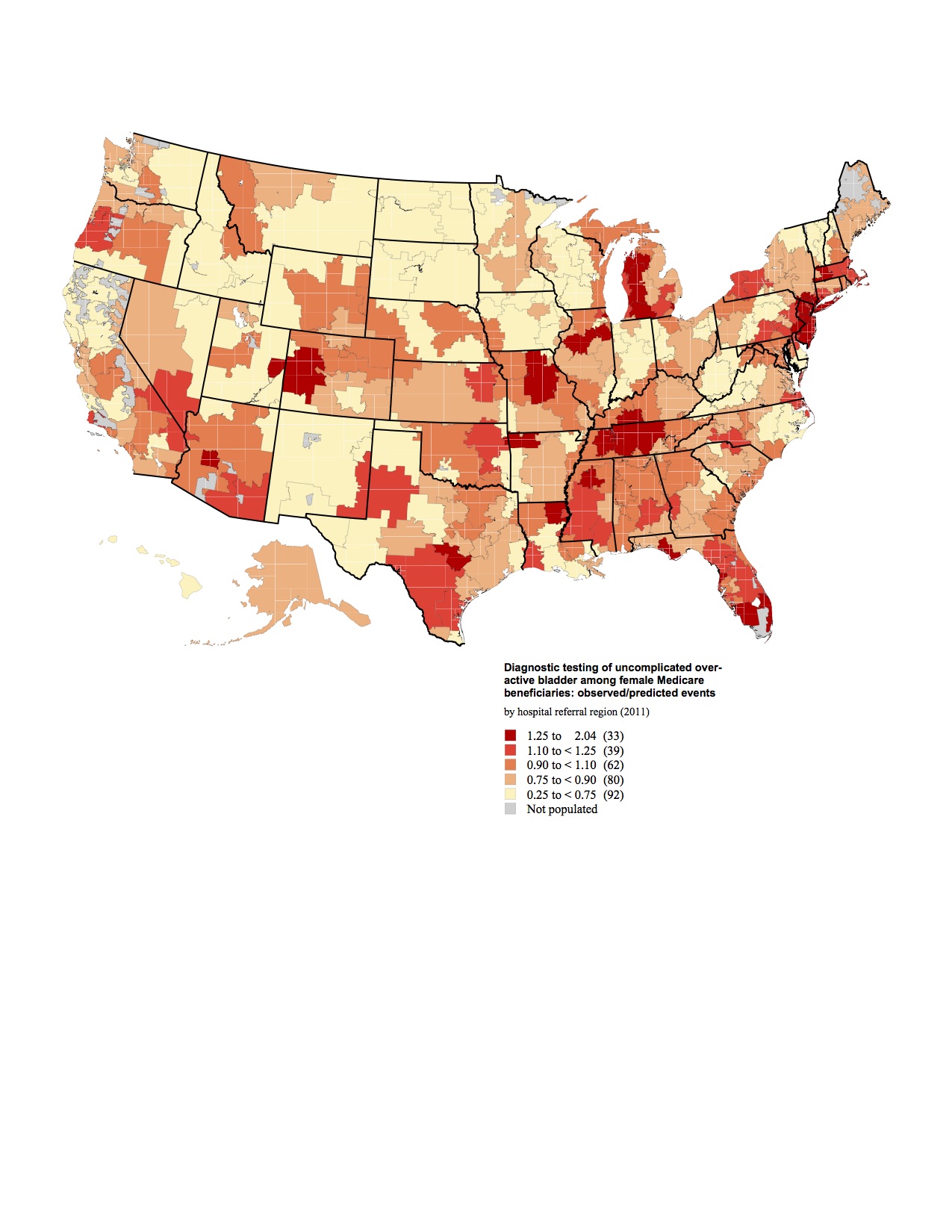
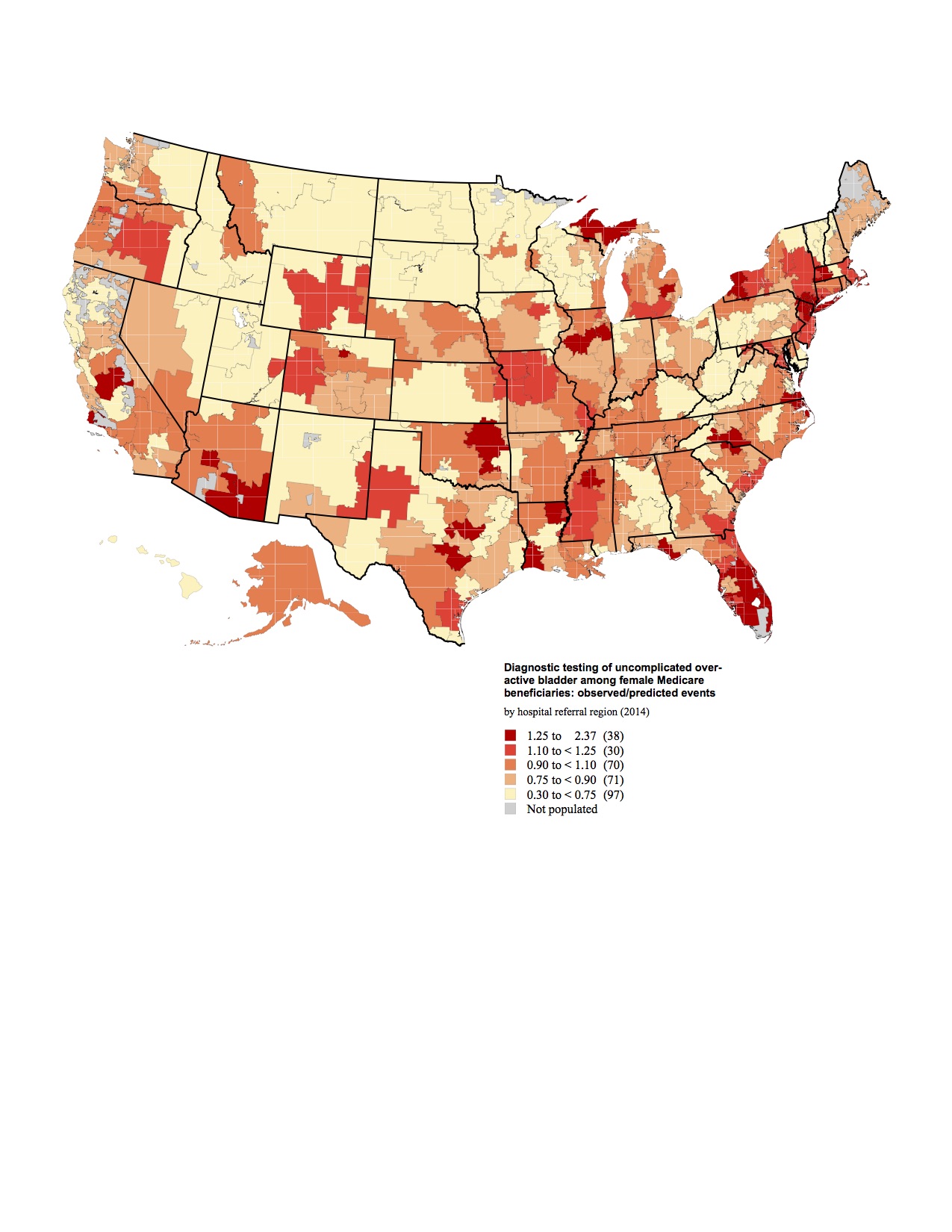
The national average rate for potentially unnecessary diagnostic procedures performed on patients with OAB was 41% (163,919/399,004) in 2011, and only slightly decreased to 38.2% (169,706/443,512) in 2014. Comparing HRRs to the national rate, use of diagnostic procedures demonstrated almost 8-fold variation even after controlling for age and race for both years (Figure 1, 2). In 2011 the lowest rate was identified in Minot, ND (0.260) and the highest in Fort Myers, FL (2.036). By 2014, following the widespread dissemination of the AUA guidelines, the lowest rate was identified in Rapid City, SD (0.304) and the highest again in Fort Myers, FL (2.37). Rates of additional procedures were typically highest in the southeast for both years.
Conclusion:
There is significant regional variation in the work up of OAB. Interestingly, the rates of diagnostic testing did not appear to change significantly after the publication of the AUA OAB guidelines. Further research is needed to identify how much of this diagnostic testing is inappropriate in order to decrease healthcare costs. Additionally more research is needed to explore the relationship of diagnostic testing to management outcomes.
1.
Ganz ML et al,. Economic costs of overactive bladder in the United States. Urology. 2010 Mar;75(3):526-32, 532.e1-18. doi: 10.1016/j.urology.2009.06.096. Epub 2009 Dec 29
2.
Gormley EA, Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline., et al American Urological Association; Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction. J Urol. 2012 Dec;188(6 Suppl):2455-63. doi: 10.1016/j.juro.2012.09.079. Epub 2012 Oct 24.
Back to 2017 Program
|
|
|
|