Back to 2017 Program
Analysis of Stent Omission after Uncomplicated Ureteroscopic Lithotripsy Shows Significant Cost Savings and Decreased Patient Morbidity
Paul E. Bower, MD, Danielle Velez, MD, Simone Thavaseelan, MD, Gyan Pareek, MD.
Brown University, Providence, RI, USA.
BACKGROUND: Prospective trials have shown that stent placement after ureteroscopic lithotripsy (URSL) is not necessary in all patients. As the Medicare Access and CHIP Reauthorization Act of 2015 ends fee for service payment in exchange for the Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (APMs) in 2017, financial analysis of URSL procedures is necessary. Specific indications for stent omission (SO) remain elusive, and the lack of clear indications may have a negative impact on cost of care. We sought to define indications for and the cost impact of SO.
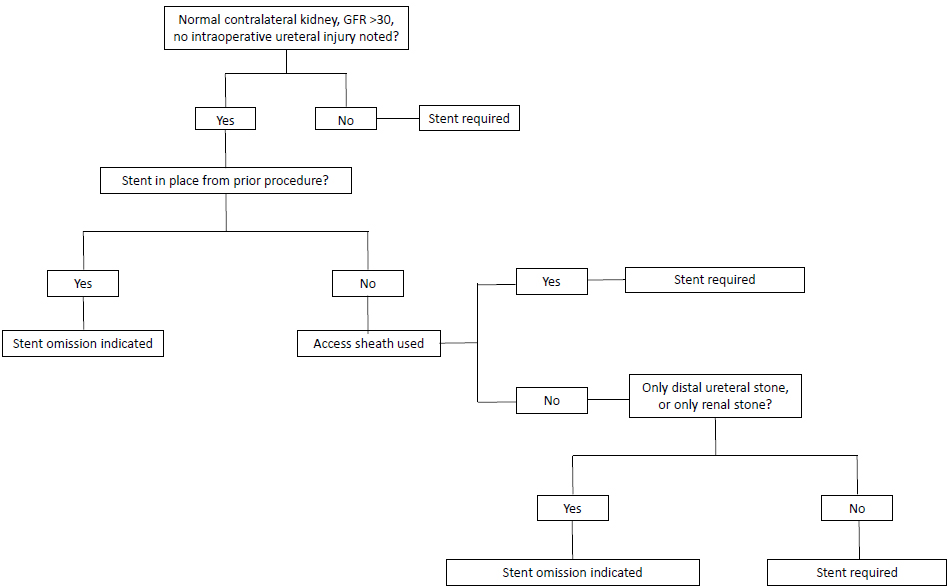
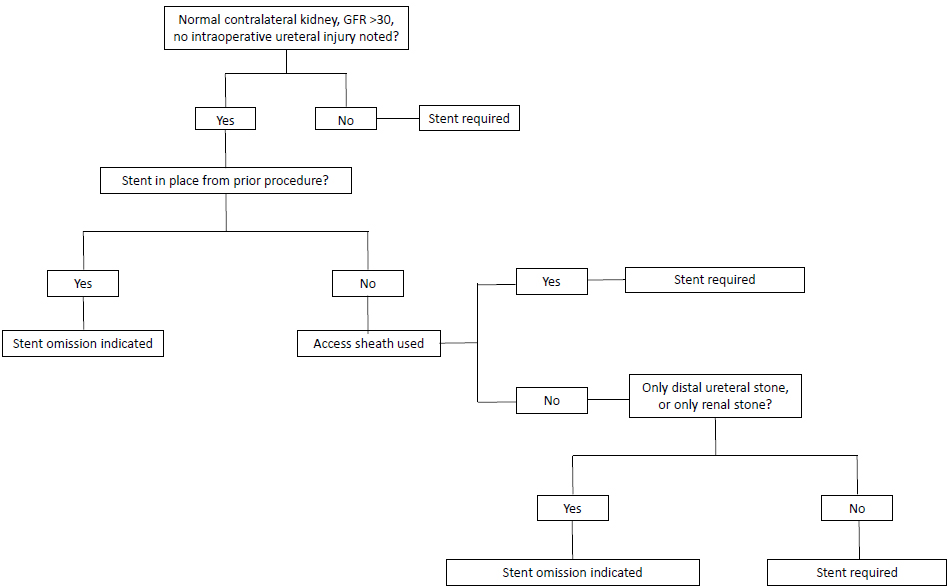
METHODS: A retrospective cohort of 126 consecutive patients who had URSL or diagnostic ureteroscopy by fellowship trained endourologists were analyzed. Indications for SO were defined according to Figure 1. Phone calls for symptoms, additional office visits, ED visits or admissions within 30 days of the procedure were recorded as postoperative events. Costs for the stent removal and from events attributable to the stent were calculated using the Medicare Physician Fee Schedule Look-Up Tool. The cost of stent placement was calculated as the cost to purchase the stent. Statistical analysis was performed using Fischer’s exact test when comparing postoperative morbidity between groups. RESULTS: SO was indicated in a total of 67 patients of the 126 analyzed, with SO performed in 9 patients. The average cost of unnecessary stent placement was $372.45 per patient, with the average cost being $540.09 for those with events and $272.92 for those without events. Annualized cost was $29,424 per endourologist. Events occurred in 23 patients with stents that were placed unnecessarily and in no patients in which SO occurred as indicated (p=0.025). Events included new flank pain, dysuria, hematuria, stent migration, and sedation for cystoscopic stent removal. CONCLUSIONS: We propose evidence based indications for SO after URSL which decrease patient morbidity and generate savings of $372.45 per patient or $29,424 annually per endourologist. These cost savings may prove vital in adjusting to new payment models.
Back to 2017 Program
|
|
|
|