Back to 2017 Program
Percutaneous Renal Access by Urologist vs Radiologist: Trends and Perioperative Outcomes in PCNL
Jacqueline M. Speed, MD1, Ye Wang, PhD1, Jeffrey J. Leow, MBBS, MPH1, Tyler R. McClintock, MD, MS1, Naeem Bhojani, MD2, Quoc-Dien Trinh, MD1, Steven L. Chang, MD, MS1, Ruslan Korets, MD3.
1Brigham and Women's Hospital, Boston, MA, USA, 2Universite de Montreal, Montreal, QC, Canada, 3Veterans Affairs Boston Healthcare System, Harvard Medical School, Boston, MA, USA.
BACKGROUND:
Percutaneous nephrolithotomy (PCNL) is an effective minimally invasive technique for removal of large upper urinary tract calculi. The initial step in percutaneous nephrolithotomy is access to the renal calyceal system via a percutaneous approach. Historically, interventional radiologists have obtained renal access; however, urologist-acquired access is feasible and appropriate in most cases. The aim of the study was to examine temporal trends of renal access by physician specialty, and to evaluate the impact of the specialty of the physician obtaining access on length of stay (LOS), complications, and costs of PCNL
METHODS:
We used data from a national hospital discharge database to identify patients who underwent PCNL between 2003-2015. Procedure codes related to renal access were linked to physician specialty. We examined patient demographics, Charlson comorbidity index, postoperative complications, LOS, and direct hospital costs. We also investigated hospital and surgeon characteristics stratified by specialty of the physician obtaining renal access. Logistic regression was used to identify trends in access acquisition. A multivariable regression model was created adjusting for potential confounders to examine complications, costs, and LOS.
RESULTS:
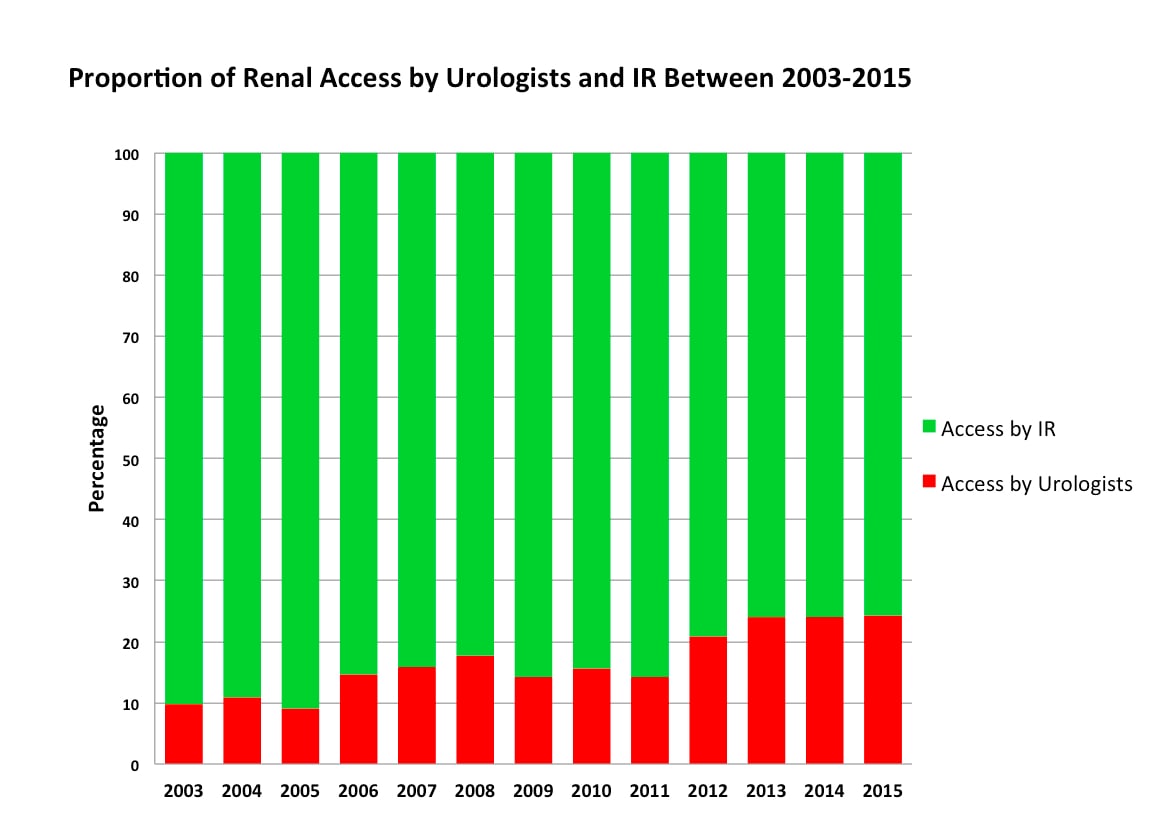
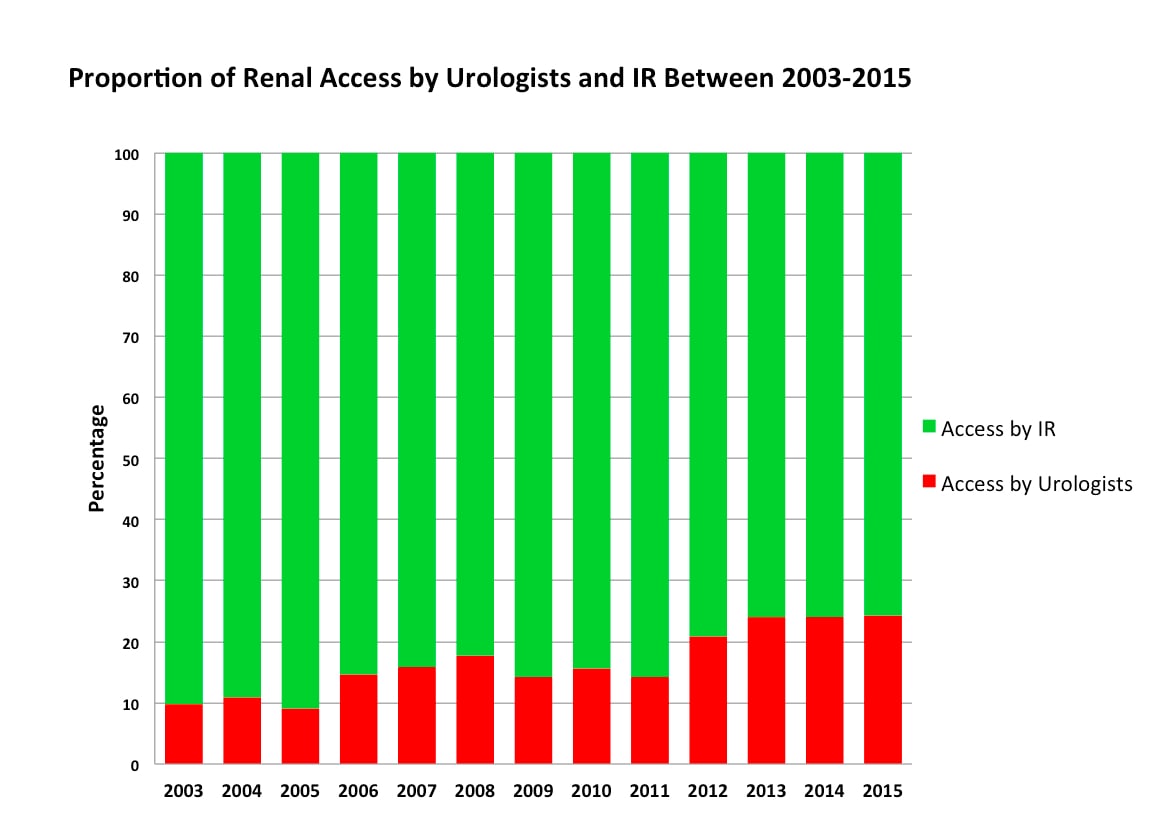
We identified 19,976 patients undergoing PCNL between 2003-2015. The proportion of urologist- obtained access increased over time (Figure 1) with 9.8% of patients having percutaneous renal access attained by urologists in 2003, compared to 24.3% in 2015 (p for trend <0.001). High volume urologists were more likely to obtain their own access (36.5% vs. 9.7% p<0.001). Renal access by urologists was associated with a lower 90-day complication rate (15.2% vs. 17.0% p=0.008) and lower rates of prolonged hospitalization ≥4 days (9.3% vs. 13.4%, p<0.001). On multivariable analysis, renal access by urologist was associated with lower rates of any complication (Clavien 1-5) (OR 0.86, p=0.006), shorter LOS (<4 days) (OR 0.71, p<0.001), and lower direct hospital costs (OR 0.83, p<0.001).
CONCLUSIONS:
In the United States, radiologists obtain percutaneous renal access in the majority of PCNLs. Though the majority of access for PCNLs continues to be done by radiologists, there is an increasing proportion of renal access for PCNL being acquired by urologists. Access by urologist may be associated with lower overall complications, shorter hospitalizations, and lower direct hospital costs. Coding errors and absence of stone complexity information may limit the cogency of our findings and requires further investigation.
Back to 2017 Program
|
|
|
|
|