Back to 2017 Program
Patient Navigation and Its Association with Treatment Selection for Low-Risk Prostate Cancer
Emily C. Serrell, MS1, Moritz H. Hansen, MD1, Gregory J. Mills, BA1, Tracy Robbins, MS2, Andrew Perry, BS2, Melanie Feinberg, BS2, Scot Remick, MD2, Lisa T. Beaule, MD2, Matthew Hayn, MD2, Tom Kinkead, MD2, Paul Han, MD, MPH1, Jesse D. Sammon, DO1.
1Center for Outcomes Research and Evaluation, Portland, ME, USA, 2Maine Medical Center, Portland, ME, USA.
BACKGROUND: Patient navigation (PN) has many theoretical and reported benefits in cancer care, including improved access to and coordination of care. In 2008, our large multi-institution health system developed a PN program to achieve these goals and to promote shared decision-making in the treatment of prostate cancer (PCa) by an independent nurse navigator. Coinciding with the implementation of our program, active surveillance had become an increasingly accepted low-risk PCa management modality, with reported national rates of about 50% by 2014. We hypothesized that our navigation program, with its emphasis on patient-centered decision-making, would be associated with increased utilization of active surveillance in men with National Comprehensive Cancer Network (NCCN) low-risk disease.
METHODS: Data were collected from our Multi-institution tumor registry from 2009 to 2015. Patients with unknown staging, node positive, and metastatic disease were excluded. A subset of patients with NCCN very-low/ low-risk disease were extracted (clinical stage ≤ T2a, Gleason score ≤ 6, serum PSA <10ng/mL). Multivariable logistic regression analyses were performed to determine factors associated with decision to use active surveillance as initial treatment, controlling for year and age at diagnosis, race, primary payer, marital status, tobacco use, urologist volume, distance from treatment facility, ZIP Code based income, and PCa characteristics (Gleason score, PSA, clinical stage, NCCN risk group).
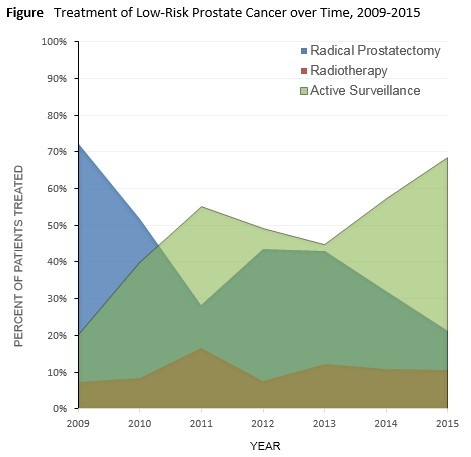
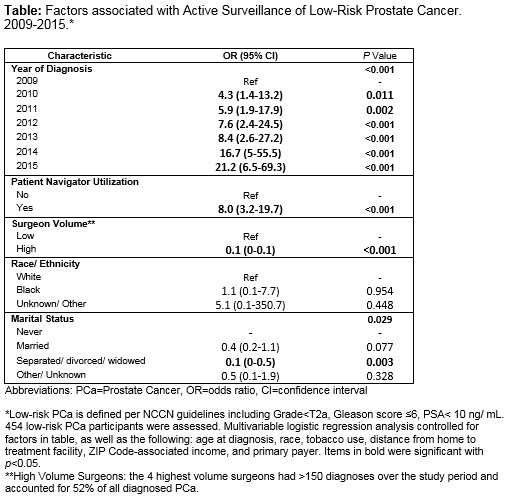
RESULTS: Data from 1,533 patients with local PCa in 2009-2015 were reviewed and treatment types assessed. Of these, 454 men had very-low/ low-risk disease. In this population over the study period, 193 men underwent radical prostatectomy and 213 chose active surveillance as initial treatment. Active surveillance increased from 20% in 2009 to 68% in 2015 (Figure). Following adjustment, patients were significantly more likely to choose active surveillance if they were navigated, treated later, treated by a low-volume surgeon, or never married (Table). Distance from care was not associated with treatment choice. Approximately 90% utilized navigation services, and PN was independently associated with active surveillance (Odds Ratio (OR)=8.0, 95% Confidence Interval (CI) 3.2-19.7).
CONCLUSIONS: Active surveillance as initial treatment modality for men with low-risk prostate cancer increased over the study period. Patient navigation was significantly associated with active surveillance. This may reflect increased decision support provided by the clinical patient navigator, who acts as an independent entity facilitating consults between multiple disciplines, educating patients and families based on NCCN guidelines, and focusing on shared decision making in treatment discussions. This may reflect changing practice patterns, as well as community perception as active surveillance became more common over the study period.This study demonstrates that navigation services may help to increase active surveillance for low-risk disease. More research is necessary to evaluate long-term patient satisfaction with treatment decision.
Back to 2017 Program
|
|
|
|
|