Back to 2025 Abstracts
Socioeconomic Status and Mortality in Fournier's Gangrene
Emma Laquinta, BA1, Allegra Rollo, BA
1, Aaron M. Seto, BA
1, Taylor Braunagel, MS
1, Kamil Malshy, MD
2, Madeline Cancian, MD
1.
1The Minimally Invasive Urology Institute, The Miriam Hospital, Warren Alpert Medical School of Brown University, Providence, RI, USA,
2University of Rochester Medical Center, Rochester, NY, USA.
Socioeconomic Status and Mortality in Fournier’s Gangrene
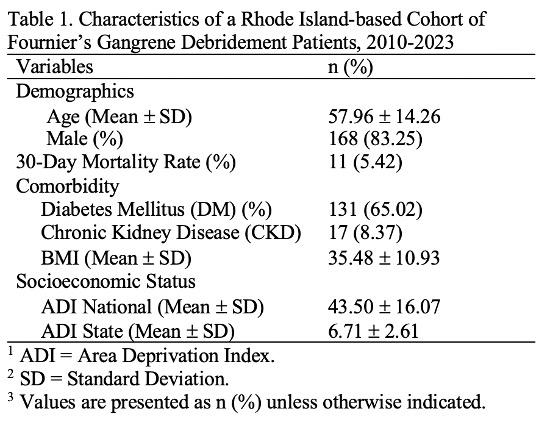
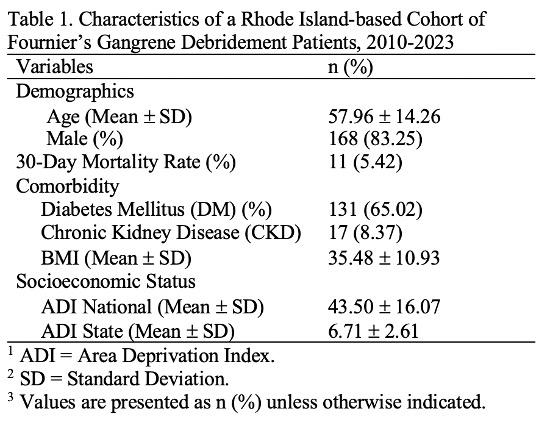
BackgroundSocioeconomic status (SES) is a known determinant of health, yet its impact on short-term mortality following hospitalization remains understudied. The Area Deprivation Index (ADI), a validated neighborhood-level SES metric (range 1-10, higher scores indicate greater deprivation), is used to assess the relationship between SES and 30-day mortality in Fournier’s Gangrene (FG), a rare but life-threatening necrotizing soft tissue infection. Given FG’s rapid progression and high mortality, understanding socioeconomic factors in survival is critical.
Materials and Methods A retrospective cohort study was conducted at Rhode Island Hospital (2010–2023). FG patients were identified based on clinical and imaging findings. Patients undergoing surgical debridement were included. State and national ADI scores were assigned using the Neighborhood Atlas, ranking zip codes by income, education, employment, and housing. Charlson Comorbidity Index (CCI) scores were calculated. Multivariate logistic regression assessed the association between ADI and 30-day mortality, adjusting for age, CCI, diabetes mellitus (DM), chronic kidney disease (CKD), and body mass index (BMI).
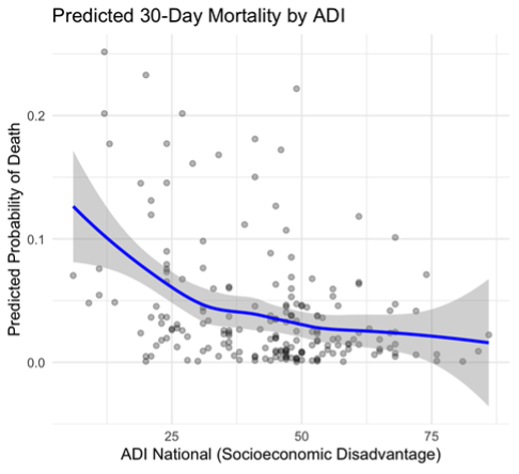
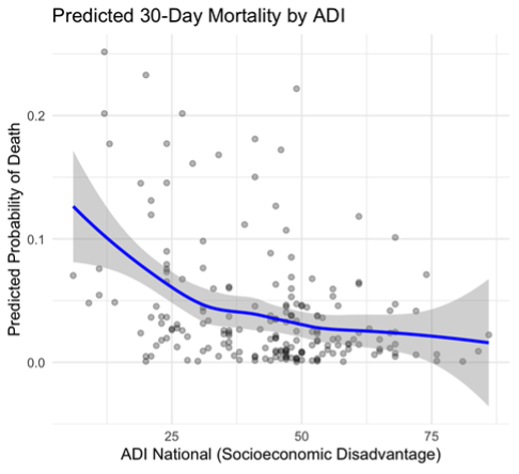
Results Among 203 FG patients (168 male), the mean state ADI was 6.76. While ADI alone did not predict 30-day mortality, the multivariate model suggested lower short-term mortality at higher ADI scores. A significant ADI-CCI interaction suggested that patients with similar comorbidity profiles had improved survival in more disadvantaged neighborhoods.
Conclusions Lower ADI (less disadvantaged SES) was associated with higher 30-day mortality, highlighting the importance of neighborhood-level SES in survival. Further research should explore protective mechanisms and health equity initiatives.
Back to 2025 Abstracts