Back to 2025 Abstracts
Does Peripheral Nerve Block prior to mini Percutaneous Nephrolithotomy Impact Opioid Requirements?
Ankur Ushir Choksi, MD1, Olamide Olawoyin, MD
1, Mursal Gardezi, MD
1, Clark Judge, MD
2, Ganesh Sanekommu, MD
1, Jinlei Li, MD
1, Piruz Motamedinia, MD
1.
1Yale School of Medicine, New Haven, CT, USA,
2MaineHealth, Portland, ME, USA.
BACKGROUND: Peripheral nerve blocks (PNBs) are increasingly utilized for intra-operative multimodal analgesia. We assessed the overall opioid requirements (OMEs), for patients that underwent mini-PCNL with PNB compared to those that were administered local anesthetic.
METHODS: We analyzed patients who underwent mini-PCNL between October 2021 and October 2024. Patients with a history of chronic pain treated with opioids, pediatric and transplant patients, and patients with Clavien-Dindo grade 2 or higher complication were excluded. Opioid administration was categorized as intra-operative, post-operative, and discharge. Patient demographics and opioid administration were compared. Continuous variables were compared using Mann-Whitney U test and continuous variables were compared using Pearson chi-squared test.
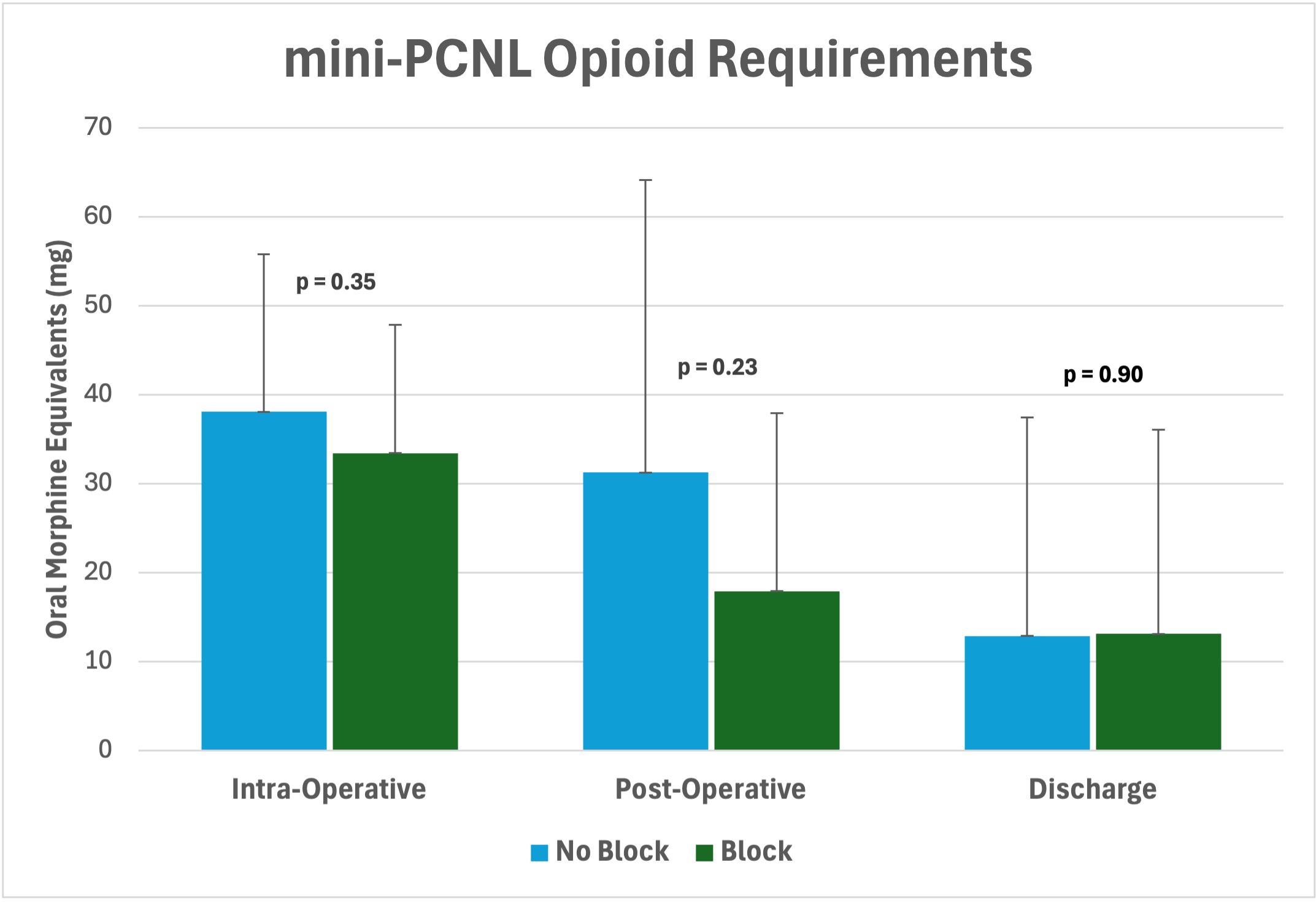
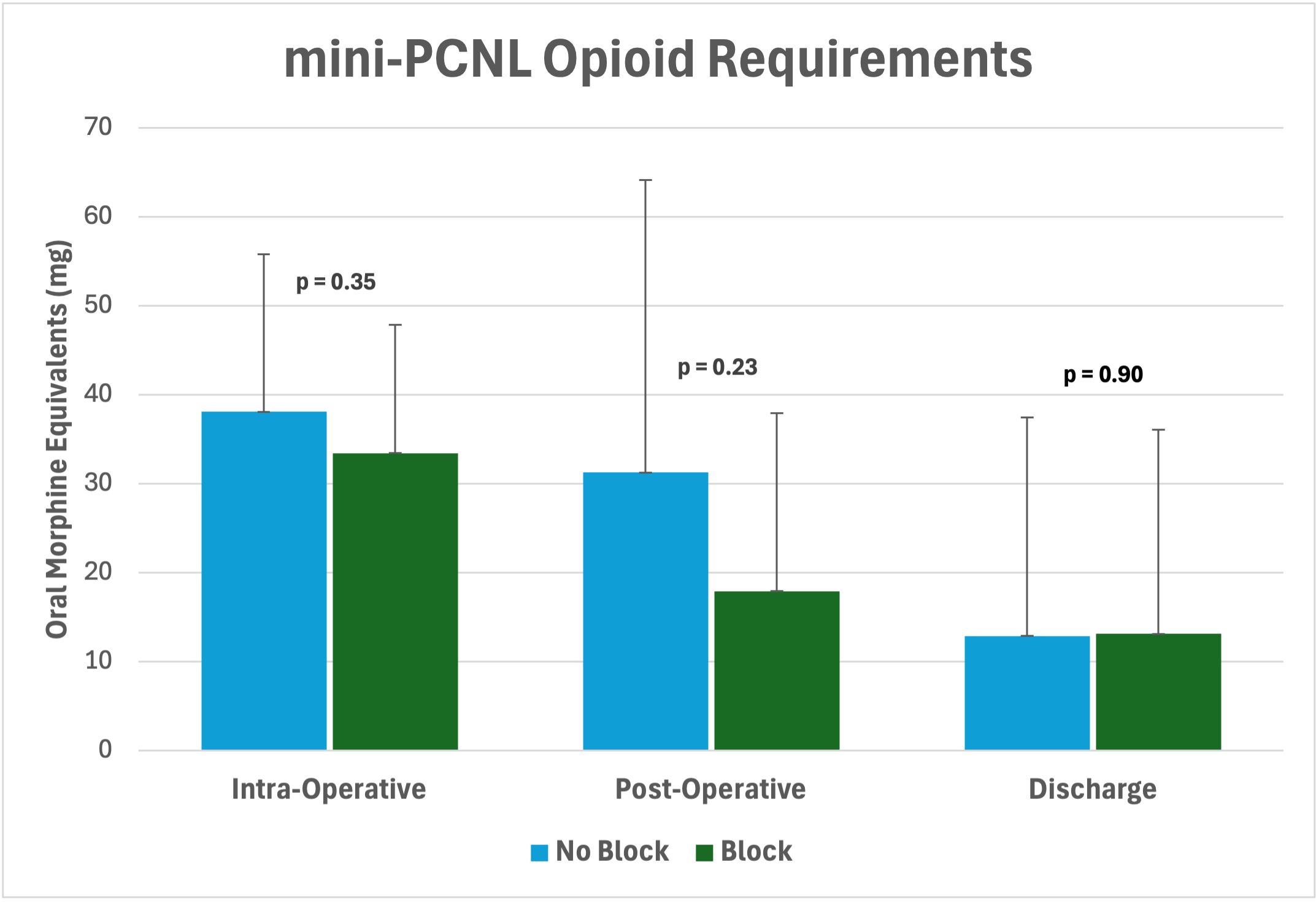
RESULTS: A total of 59 patients were retrospectively analyzed of which 45 patients had received a PNB and 14 patients did not. Of those that received a PNB, 42 received an erector spinae block and 3 received a quadratus lumborum block. Patient demographics were similar between those that did and did not receive a PNB with respect to age, sex, race, body mass index, and comorbidities (Table 1). Operative duration was similar but length of stay was longer for patients who did not receive a PNB (p = 0.007). Total opioid administration (p = 0.19) was similar between the two groups as well as intra-operatively, post-operatively and on discharge (Table 1). Toradol administration was similar between the two groups (p= 0.32).
CONCLUSIONS: For patients undergoing mini-PCNL, peripheral nerve block was associated with shorter length of stay andsimilar opioid administration compared to local anesthetic.
| Variable | | All | | Local Anesthetic | | Peripheral Nerve Block | | p-value |
| Count | | 59 | | 14 | | 45 | | |
| Age | | 59.1 ± 14.5 | | 62.5 ± 14.6 | | 58.0 ± 14.4 | | 0.22 |
| Sex, male (%) | | 34 (57.6%) | | 7 (50.0%) | | 27 (60.0%) | | 0.51 |
| Race | | | | | | | | 0.39 |
| Caucasian | | 33 (55.9%) | | 8 (57.1%) | | 25 (55.6%) | | |
| Black | | 10 (16.9%) | | 4 (28.6%) | | 6 (13.3%) | | |
| Hispanic | | 12 (20.3%) | | 1 (7.1%) | | 11 (24.4%) | | |
| Other | | 4 (6.8%) | | 1 (7.1%) | | 3 (6.7%) | | |
| Charleson Comorbidity Index | | 1.2 ± 1.9 | | 1.2 ± 2.1 | | 1.2 ± 1.8 | | 0.98 |
| BMI (kg/m²) | | 30.8 ± 6.1 | | 29.0 ± 5.9 | | 31.4 ± 6.0 | | 0.26 |
| Operative Duration (min) | | 115.0 ± 44.9 | | 102.7 ± 20.6 | | 118.8 ± 49.5 | | 0.64 |
| Length of Stay (hours) | | 14.1 ± 12.1 | | 25.0 ± 14.5 | | 10.8 ± 9.1 | | 0.007 |
| Ketorolac Administration | | 19 (32.2%) | | 3 (21.4%) | | 16 (35.6%) | | 0.32 |
| | | | | | | | | |
| Intra-operative OME (mg) | | 39.6 ± 38.3 | | 59.6 ± 72.6 | | 33.4 ± 14.6 | | 0.20 |
| Post-operative OME (mg) | | 21.1 ± 24.4 | | 31.2 ± 32.9 | | 17.9 ± 20.0 | | 0.23 |
| Discharge OME (mg) | | 13.1 ± 23.3 | | 12.9 ± 24.6 | | 13.1 ± 22.9 | | 0.90 |
| Total OME (mg) | | 73.7 ± 61.9 | | 86.4 ± 59.1 | | 64.4 ± 39.7 | | 0.19 |
| Patient call for pain with opioid prescribed | | 3 (5.1%) | | 2 (14.3%) | | 1 (2.2%) | | 0.07 |
Back to 2025 Abstracts