Back to 2025 Abstracts
Infection Rates with Intraoperative Dilute Chlorhexidine Gluconate in Hydrophilic Coated Inflatable Penile Implants: Initial Results from a Large Multi-Institutional Cohort
Richard Hans Bellemare, MD1, Samuel Ivan, MD
2, Muhammed AM Hammad, MBBCh
3, Elia Abou Chawareb, MD
3, Faysal A. Yafi, MD
3, Helen L. Bernie, MD
4, Aaron C. Lentz, MD
5, Paul Perito, MD
6, Charles Welliver, MD
7, Paul H. Chung, MD
8, Tung-Chin Hsieh, MD
9, Allen F. Morey, MD
10, Sevann Helo, MD
11, Matt J. Ziegelmann, MD
11, Jonathan N. Warner, MD
11, Tobias S. Kohler, MD
11, Hossein Sadeghi-Nejad, MD
12, Sarah Vij, MD
13, Petar Bajic, MD
14, Kelli Gross, MD
15, James Hotaling, MD
15, Martin S. Gross, MD
1, Jay Simhan, MD
2.
1Dartmouth Hitchcock Medical Center, Lebanon, NH, USA,
2Fox Chase Cancer Center, Philadelphia, PA, USA,
3University of California, Irvine, Orange, CA, USA,
4Indiana University, Indianapolis, IN, USA,
5Duke University, Raleigh, NC, USA,
6Perito Urology, Coral Gables, FL, USA,
7Albany Medical Center, Albany, NY, USA,
8Jefferson Health, Philadelphia, PA, USA,
9University of California, San Diego, La Jolla, CA, USA,
10Urology Clinics of North Texas, McKinney, TX, USA,
11Mayo Clinic, Rochester, MN, USA,
12New York University, New York, NY, USA,
13University of Texas, Austin, Austin, TX, USA,
14Cleveland Clinic, Cleveland, OH, USA,
15University of Utah, Salt Lake City, UT, USA.
BACKGROUND: Dilute 0.05% Chlorhexidine Gluconate (CHG) has increasing use as irrigation for inflatable penile prosthesis (IPP) surgery. There is conflicting in vitro data on CHG use with hydrophilic coated devices. We assessed infection rates for hydrophilic coated devices with intraoperative CHG use in a large multi-institutional cohort.
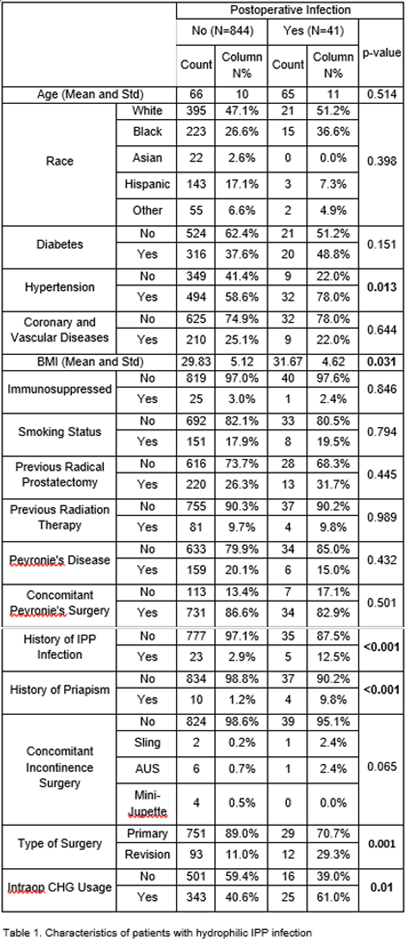
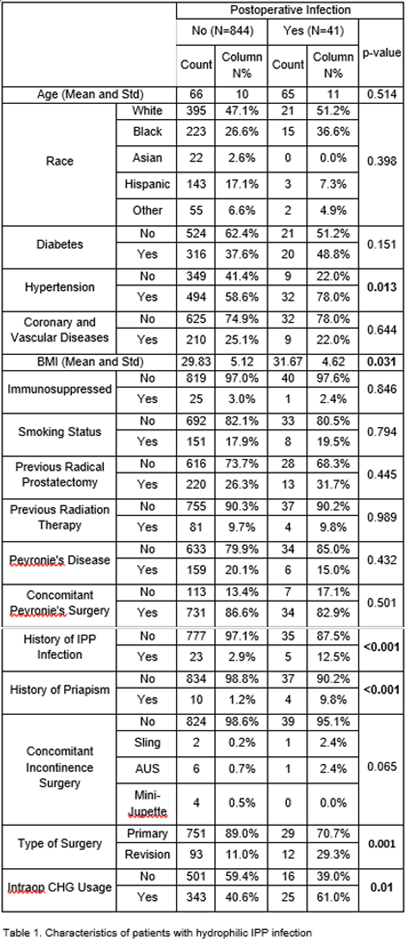
METHODS: We conducted a retrospective analysis of 1,604 patients undergoing IPP placement across 12 centers. Data collection spanned January 1, 2017 to March 1, 2024. Surgeons contributed patients who underwent IPP placement using CHG irrigation or dip, and an equal number of consecutive control patients without CHG use. The primary outcome was explant for postoperative infection. Demographics were compared using chi-squared testing. Factors associated with infection were assessed with logistic regression analysis.
RESULTS: Hydrophilic devices were placed in 885 patients. The incidence of infection with intraoperative CHG use was significantly higher than without CHG (6.8% vs.3.1%, p=0.01). Highest infection rates were seen using CHG as both irrigation and dip (7.51%, p=0.01). CHG irrigation with antibiotic dip had an infection rate of 4.39% (p=0.89). Patients with infection had higher proportions of hypertension, prior infection, priapism, revision surgery, CHG use, and higher BMI.
On multivariable logistic regression, hypertension (OR 2.15, 95%CI 1.12-5.67, p=0.026) and priapism history (OR 8.65, 95%CI 2.45-30.61, p=0.001) remained associated with increased odds of infection. CHG use was significant on univariate analysis but not multivariable analysis (OR 1.64, 95%CI 0.83-3.26, p=0.157).
CONCLUSIONS: In a large multi-institutional cohort, intraoperative CHG use was associated with an elevated incidence of hydrophilic IPP infection. This association was seen in chi-squared testing and univariate analysis but was not significant on multivariable analysis, indicating that additional power is needed to clarify these findings.
Back to 2025 Abstracts