Back to 2025 Abstracts
Urodynamic Outcomes Following Photovaporization of the Prostate for Benign Prostatic Hyperplasia: Diminished Detrusor Voiding Pressure Preserves Function After Surgery
Jonathan S. Kim, Medical Student1, Parker J. Simpson, Independent Researcher
2, Chaimaa M. Hossaini, Independent Researcher
2, Louis S. Liou, MD, PhD
3.
1Drexel University College of Medicine, Philadelphia, PA, USA,
2AOA Urological Associates, Boston, MA, USA,
3Emerson Hospital, Concord, MA, USA.
Background: Photovaporization of the prostate (PVP) is a minimally invasive treatment for benign prostatic hyperplasia (BPH) with fewer complications than transurethral resection of the prostate. However, its precise effect on bladder function remains unclear. This study examines urodynamic changes underlying subjective improvements after PVP.
Methods: In this single-center prospective study, BPH patients with lower urinary tract symptoms underwent pre- and post-op urodynamic studies (UDS) and International Prostate Symptom Score (IPSS) assessments. UDS parameters included average flow rate (Q
avg), max flow rate (Q
max), detrusor pressure at max flow (P
detmax), and max detrusor pressure (maxP
det). The bladder outlet obstruction index (BOOI) was calculated as P
detmax-2Q
max. Each patientís pre-op subjective (IPSS score) and objective (UDS) data were compared to post-op and were compared using the Wilcoxon signed-rank test.
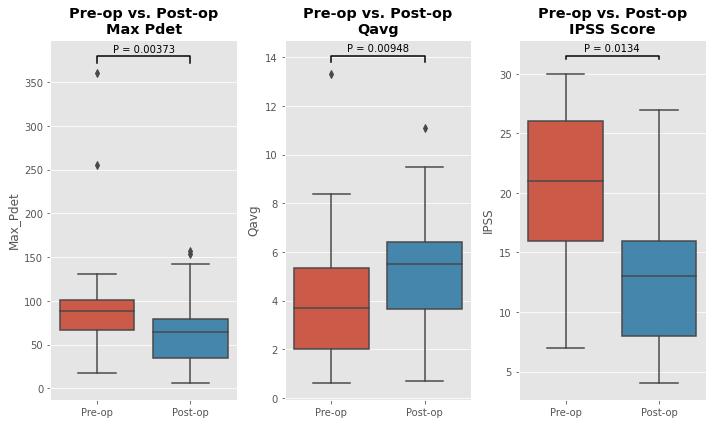
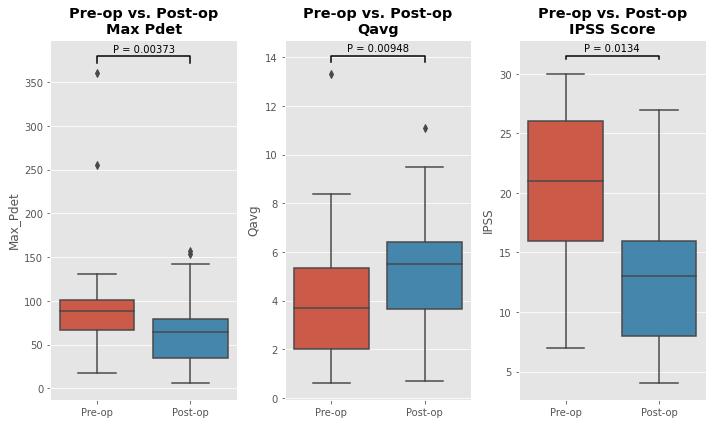
Results. Total of 23 patients were studied (mean age 71.3 years, SD = 10.2). The IPSS scores improved from pre-op (20.5) to post-op (14.2) (p=0.01). MaxP
det decreased from 102.3 to 67.1 (p<0.01), and P
detmax from 72.3 to 41.7 (p=0.02). Q
avg increased from 4.0 to 5.4 (p<0.01). Q
max remained unchanged (19.7 vs. 15.4). BOOI decreased from 43.1 to 20.1 (p=0.01).This real-world study provides insight into the urodynamic effects of PVP. Decreased max P
det and P
detmax reflect improved bladder outlet dynamics and decreased obstruction post-PVP. By allowing for lower pressure voiding, the workload of the detrusor to sustain flow decreases, enhancing efficiency. Increased Q
avg despite unchanged Q
max likely reflects more sustained flow with reduced detrusor workload and greater efficiency.
Conclusions: Though rarely performed in BPH procedures, UDS offers objective insights into bladder voiding dynamics that account for the subjective improvements seen post-surgery, and its implementation is the goal for all BPH surgeries.
Back to 2025 Abstracts