Back to 2025 Abstracts
Examining Medicare Part D Prescriber Patterns for Overactive Bladder Medications Amongst Urology Versus Non-Urology Providers in a Rural State
Architha Sudhakar, MD, Evelyn James, MPH, Sanchita Bose, MD.
Maine Medical Center, Portland, ME, USA.
Background: While anticholinergic medications are a mainstay of overactive bladder (OAB) treatment, multiple studies demonstrate their negative effects on cognition in the elderly. We investigated OAB medication prescribing patterns of urology versus non-urology providers in a rural state with a high cohort of older (>65 years) residents.
Methods: We utilized the publicly available Medicare Part D Prescribers database to identify providers prescribing OAB medications in 2022. These providers were categorized as “urology” or “non-urology” if registered as a different specialty. We compared prescribing patterns across various medications between the two groups using odds ratio and 95% confidence intervals.
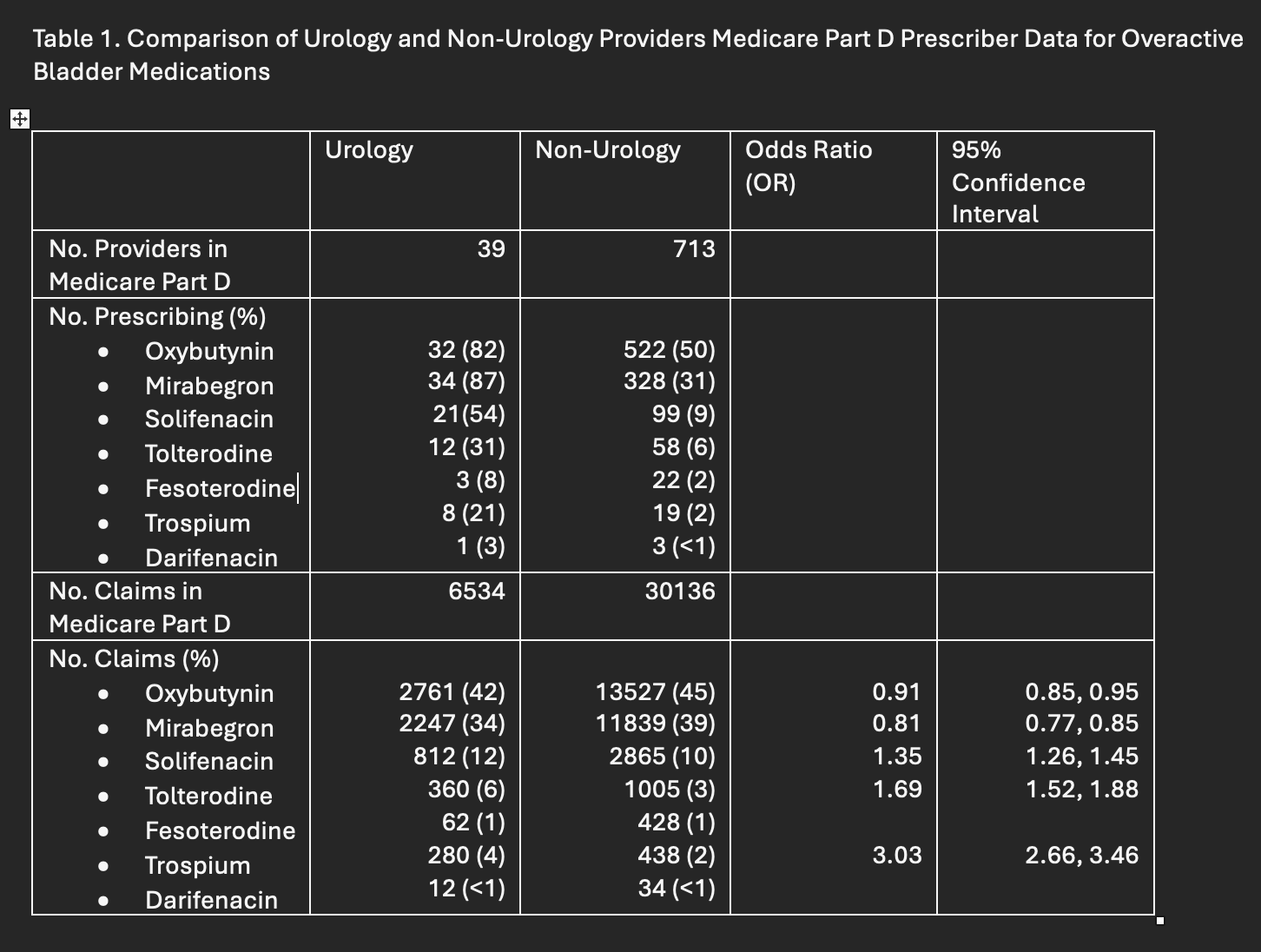
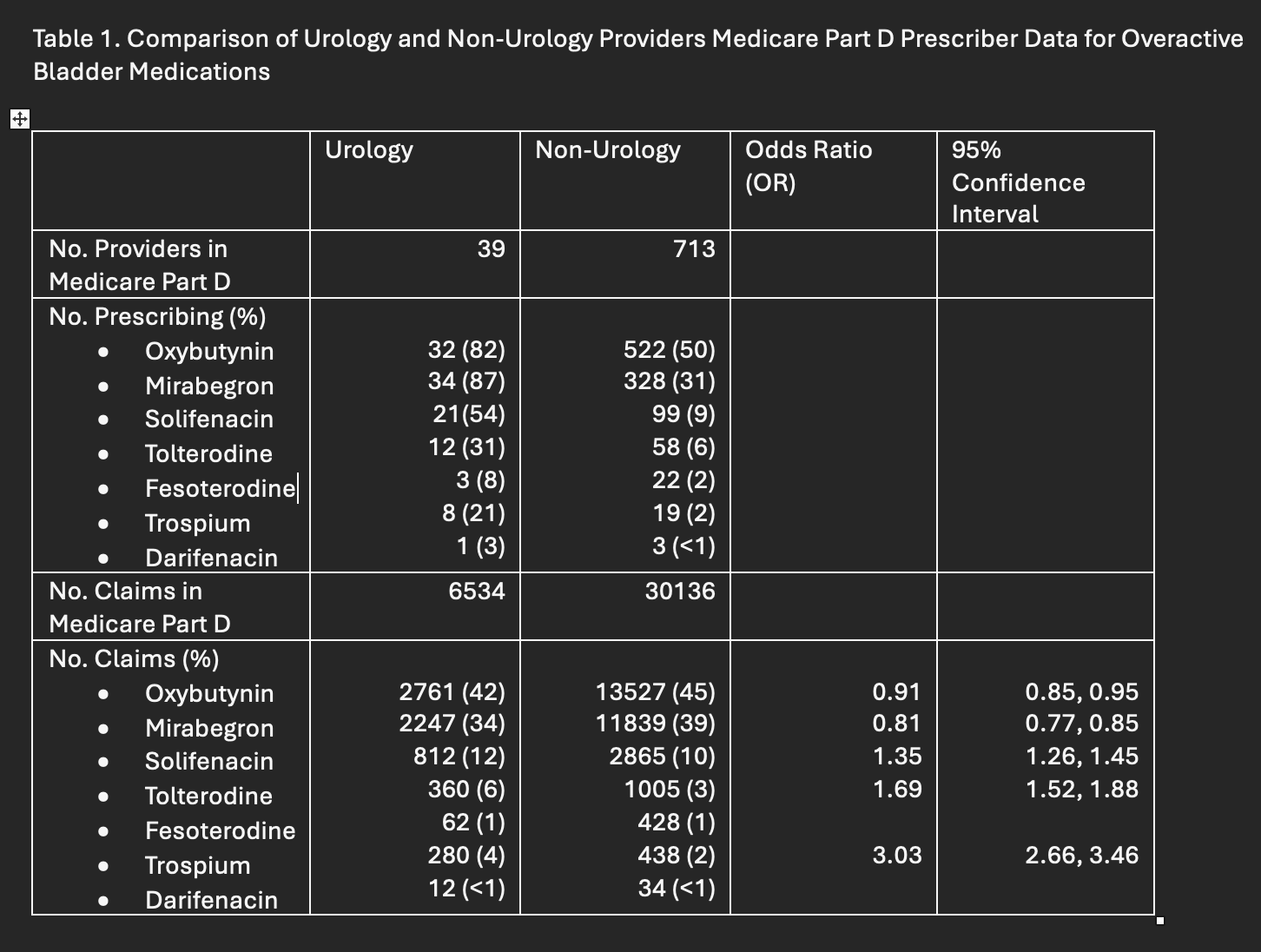
Results: Of 752 providers prescribing OAB medications, 39 (5%) were urology providers and 713 (95%) were non-urology providers (Table 1). Oxybutynin and mirabegron were the most prescribed medications across both groups (Figure 1). However, urology providers were more likely to prescribe less common agents such as solifenacin (OR= 1.35, 95% CI= 1.26, 1.45), tolterodine (OR= 1.69, 95% CI= 1.5, 1.88), and trospium (OR= 3.03, 95% CI= 2.66, 3.46) compared to their non urology counterparts (Table 1). In general, urology providers had a broader range of prescribing patterns compared to non-urology providers.
Conclusions: Anticholinergic medications remain the most prescribed agents for OAB among all providers despite evidence demonstrating their negative effects. While urologists were more likely to prescribe alternative agents, they comprise a small proportion of total prescribers. More education regarding medications and alternative therapeutic strategies may be required to better inform provider and patient decision making with regards to OAB management.

Back to 2025 Abstracts