Back to 2025 Abstracts
Socioeconomic disadvantage is associated with prostate cancer diagnosis and severity in the state of Rhode Island: A study of neighborhood-based variation
Angelo Blancaflor, BS1, Tim Wynter, BS
1, Borivoj Golijanin, MD
2, Natalia Alzate, BS
2, Taylor Braunagel, MS
2, Elias Hyams, MD
2.
1The Warren Alpert Medical School of Brown University, Providence, RI, USA,
2Brown University Health, Minimally Invasive Urology Institute, Providence, RI, USA.
BACKGROUND: Socioeconomic disparities continue to influence prostate cancer (PCa) incidence and outcomes. The Area Deprivation Index (ADI) quantifies neighborhood socioeconomic disadvantage. This study assessed neighborhood-based variation in PCa severity and treatment in Rhode Island.
METHODS: A retrospective chart review was conducted on PCa patients diagnosed between 2018-2023 at The Miriam Hospital and Lifespan Cancer Institute. Clinical data included Gleason grade group, D’Amico risk score, and treatments (surgery, chemotherapy, radiation, androgen deprivation therapy [ADT]). Patients’ addresses were linked to census block groups to assign ADI levels (1 = least deprived, 10 = most deprived). Statistical analyses examined incidence by ADI, treatment likelihood, and associations between ADI and disease severity using ordinal logistic regression.
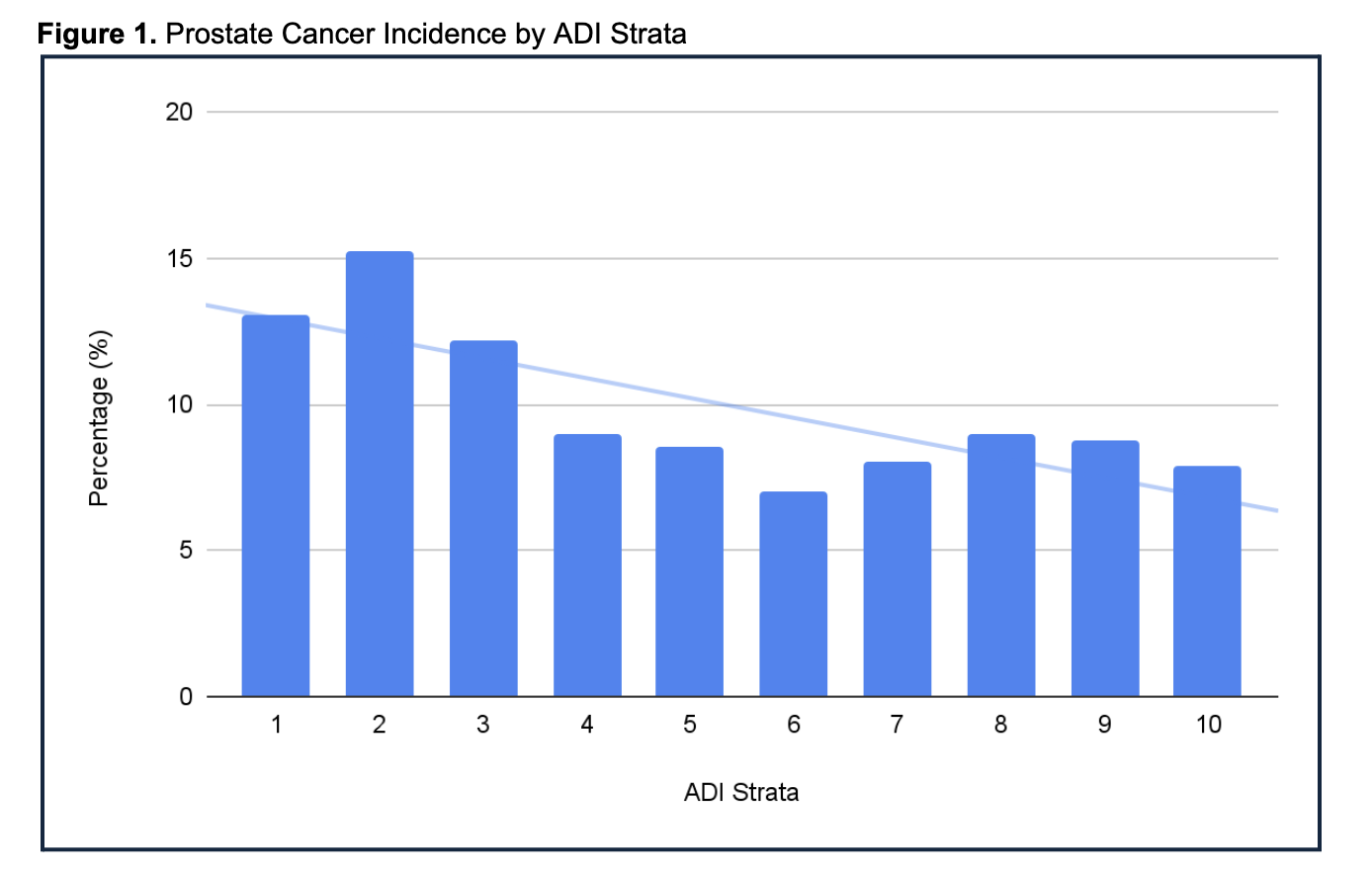
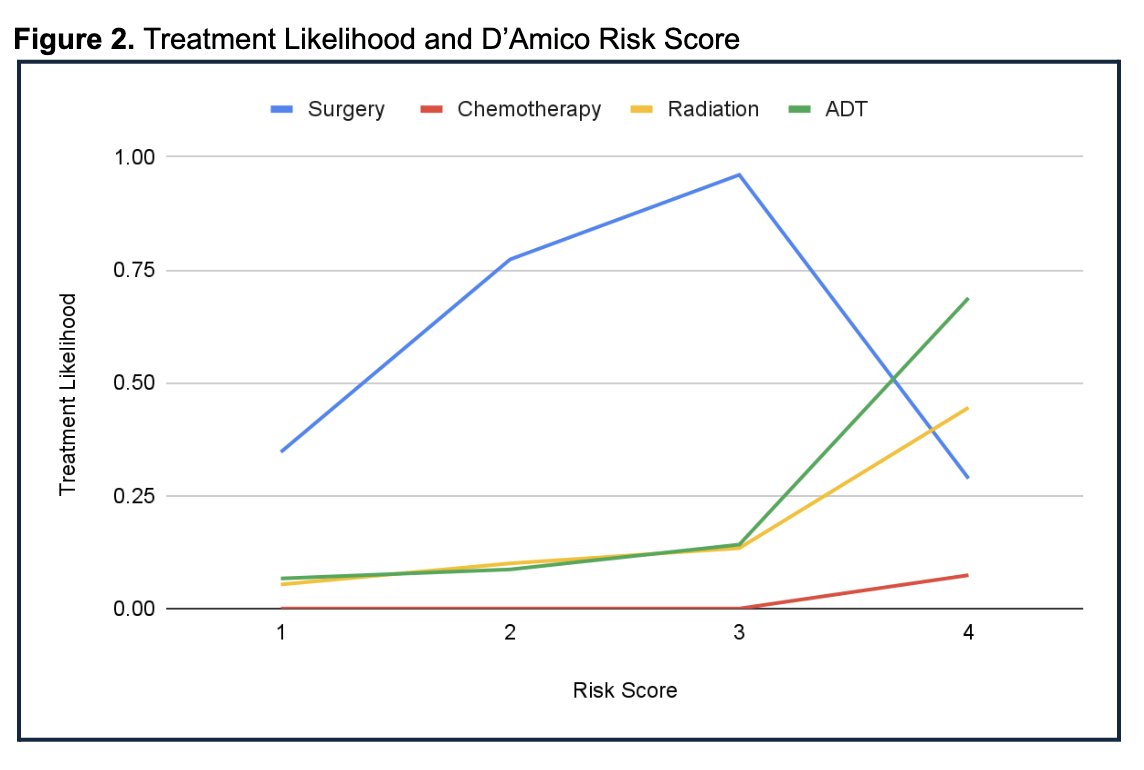
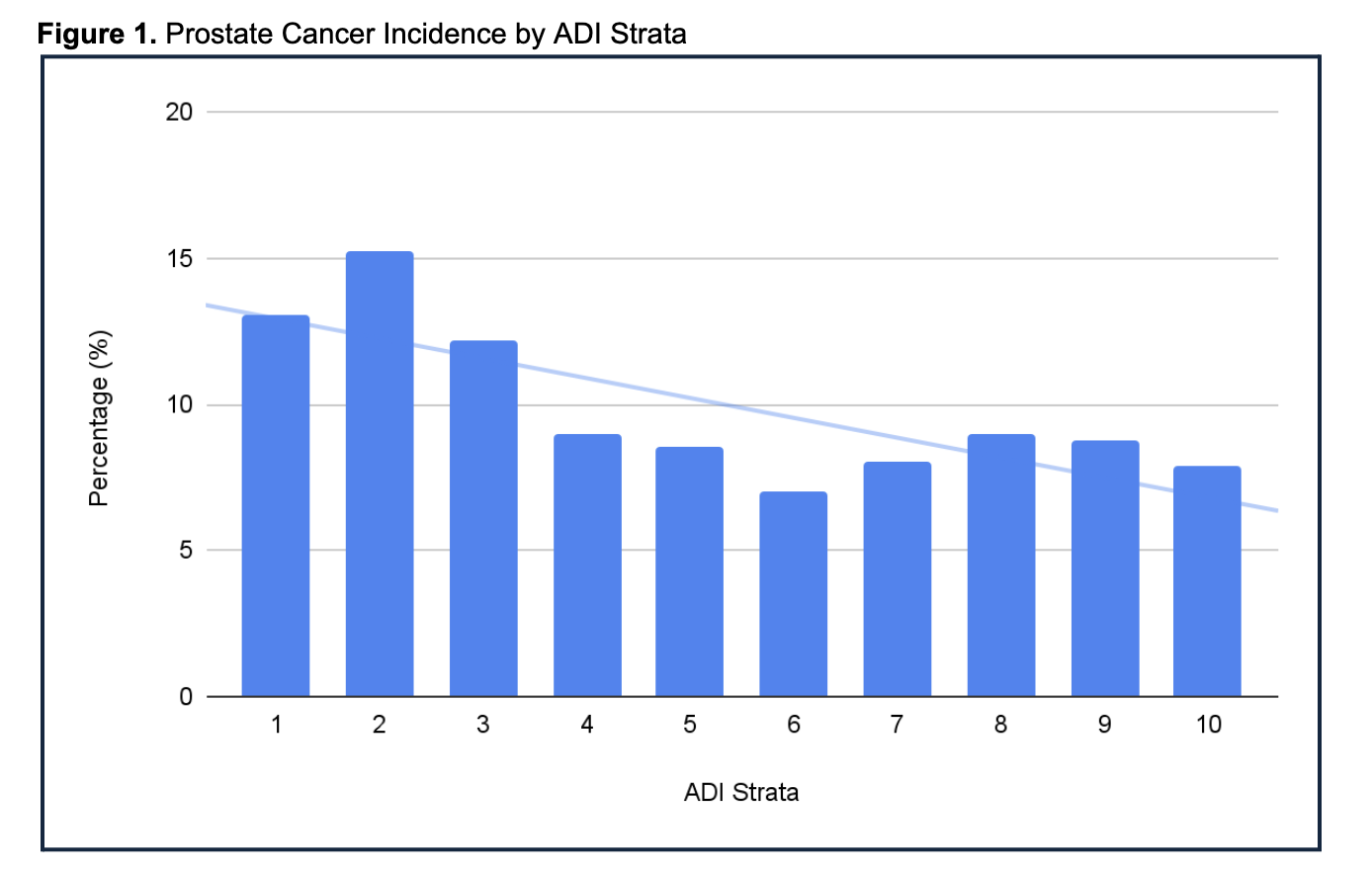
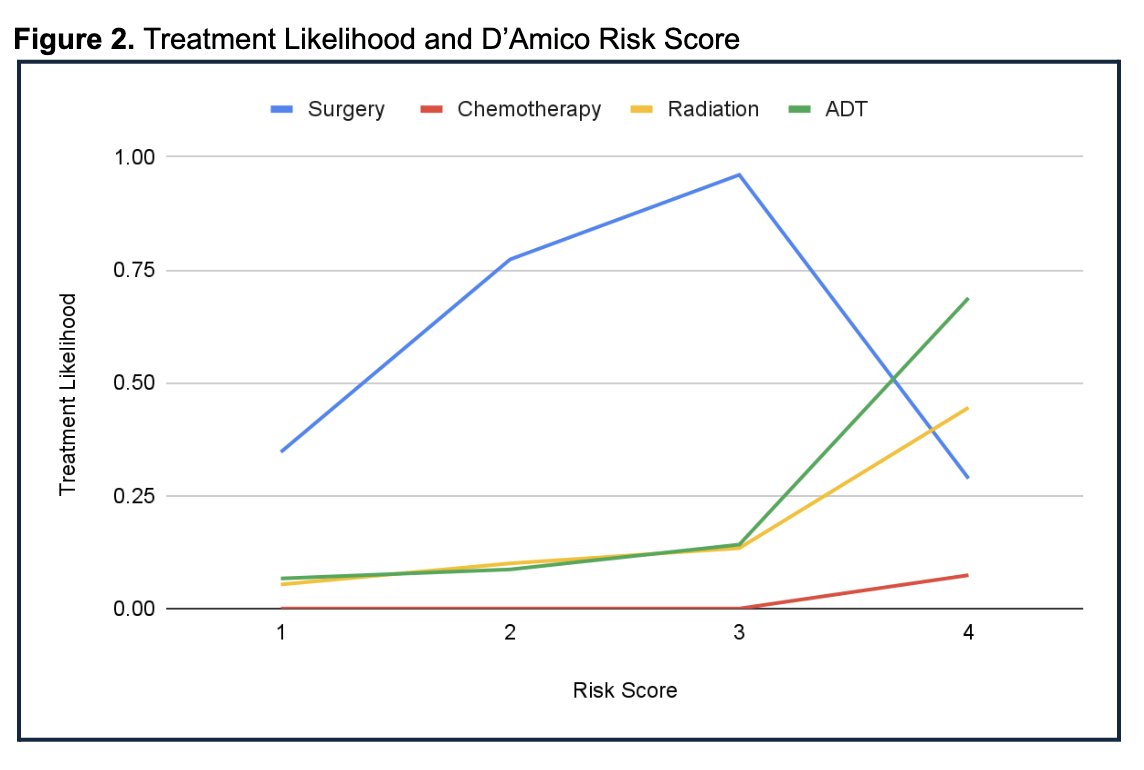
RESULTS: Analysis included 1,195 patients. PCa incidence was higher in lower ADI strata and decreased in higher strata (Figure 1). Treatment approaches were consistent across ADI levels. Treatment was associated with disease severity (Gleason and D’Amico scores) rather than socioeconomic status (Figure 2). A greater proportion of high-risk patients (D’Amico score 4) were found in higher ADI strata. Regression analysis showed a significant association between higher ADI and more severe disease (e.g., ADI 9 coefficient = 0.635, p < 0.05), with ADI 5 and 9 patients more likely to present with Gleason grade group 4-5 tumors.
CONCLUSIONS: While PCa was more common in affluent neighborhoods, disadvantaged areas had higher-risk cancers. Treatment consistency across ADI levels highlights the benefit of systematic care. Further study is needed to address disparities in detection and severity.
Back to 2025 Abstracts