Back to 2025 Abstracts
Neoadjuvant Chemotherapy and Wound Healing Complications Following Radical Cystectomy for Muscle-Invasive Bladder Cancer
Emma A. Harwood, MD1, Randie E. White, MS, MD
1, Evelyn James, MPH
1, Joshua A. Linscott, MD, PhD
2, Matthew T. Hayn, MD
1, Jesse D. Sammon, DO
1, Jeffrey M. Howard, MD, PhD
1, Stephen T. Ryan, MD
1.
1Maine Medical Center, Portland, ME, USA,
2Moffitt Cancer Center, Tampa, FL, USA.
BACKGROUND:
Neoadjuvant chemotherapy (NAC) is standard of care for eligible patients (pts) with muscle-invasive bladder cancer (MIBC), offering improved survival. However, NAC may contribute to nutritional depletion and impaired wound healing. Prior studies assessing high-grade complications after NAC and radical cystectomy (RC) have reported conflicting findings. This study examines the relationship between NAC and wound-related complications requiring intervention following RC. METHODS:
We reviewed RC cases from 2014-2024 at a high-volume statewide referral center. All pts were evaluated by multidisciplinary teams and followed for 90 days postoperatively. Patients were stratified by receipt of NAC (partial/full course vs. none). The primary outcome was high-grade wound-related complications requiring intervention. Chi-square and backward stepwise regression were used to analyze associations between NAC and complications. RESULTS:
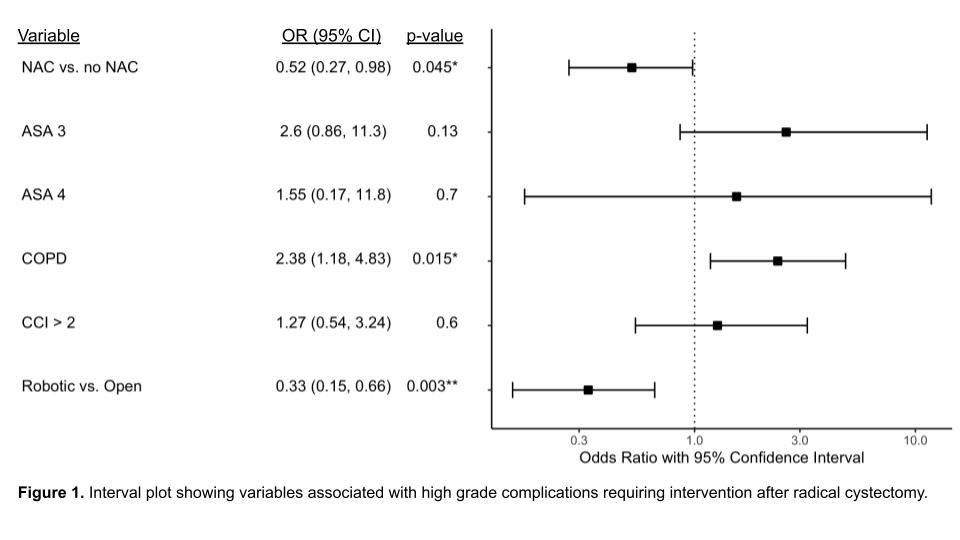
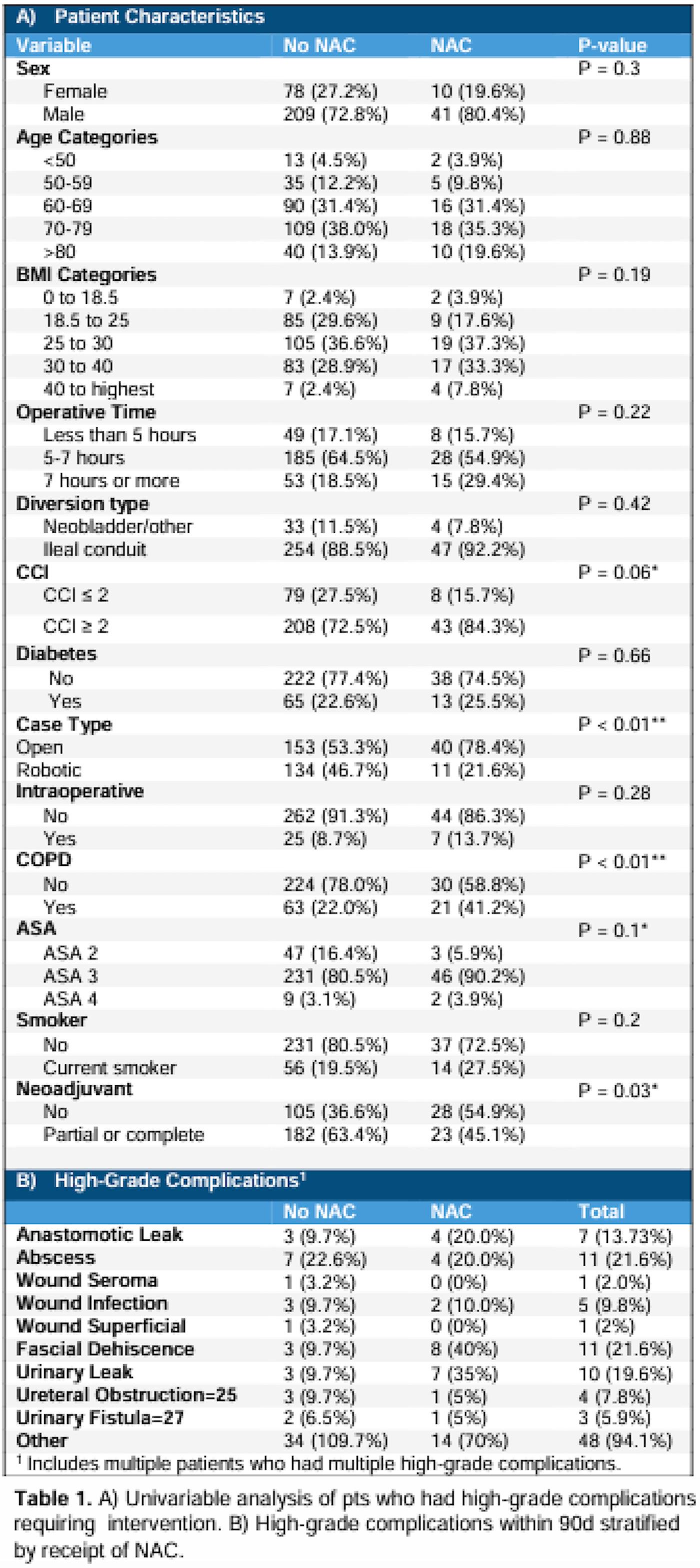
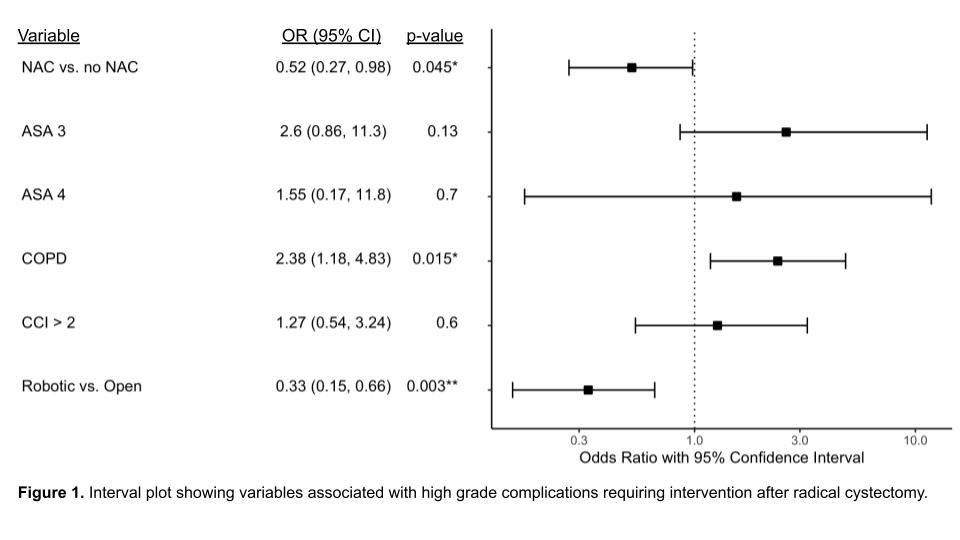
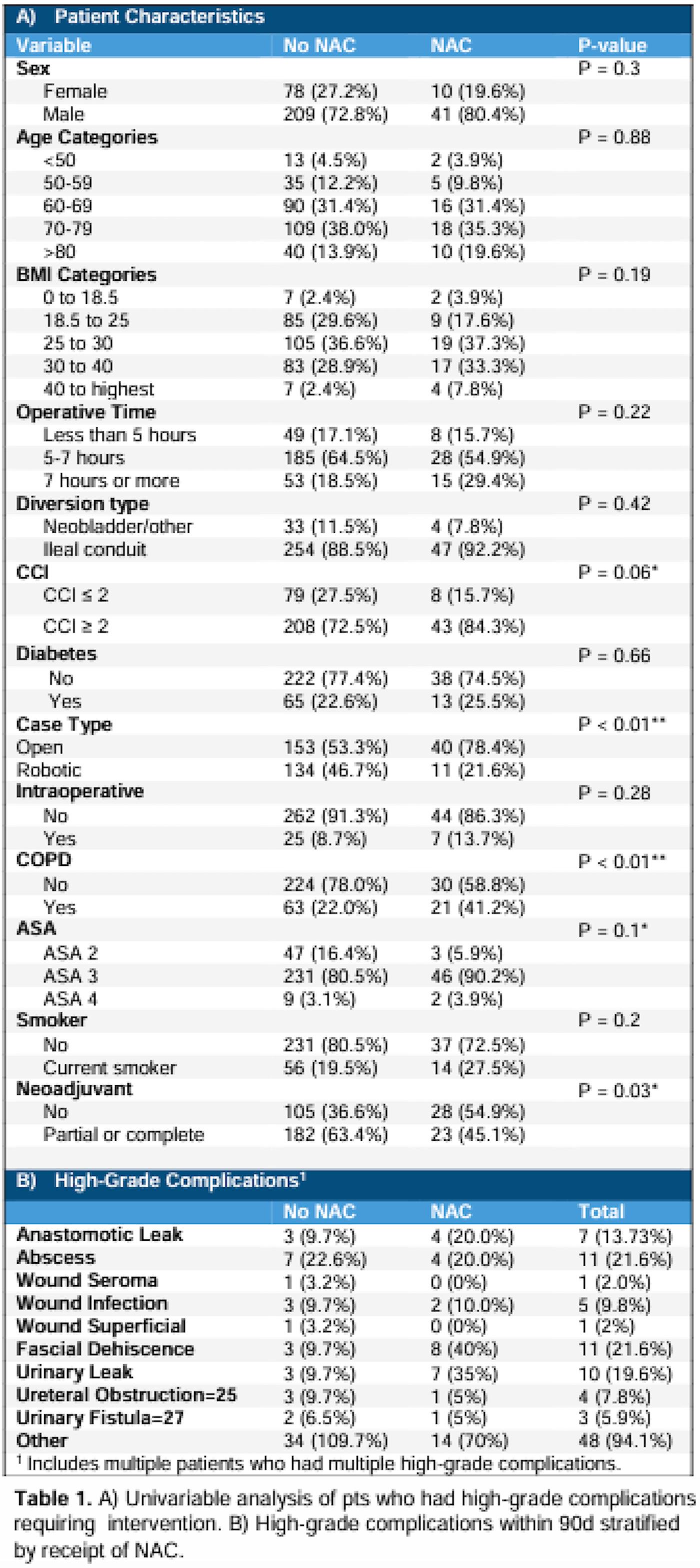
Among 338 RC pts, 205 (60.1%) received NAC. High-grade complications occurred in 20 NAC pts (9.8%). On univariable analysis, NAC, COPD, ASA score, open surgery, and CCI >2 were associated with complications (Table 1A). Multivariable analysis demonstrated that NAC was independently associated with lower odds of complications (OR 0.52, 95% CI 0.27-0.98, p=0.045, Figure 1). The most common were abscess (21.6%), fascial dehiscence (21.6%), and urinary leak (19.6%) (Table 1B). Fascial dehiscence, anastomotic leak, and urinary leak occurred more frequently in the NAC group, though not all differences reached significance. CONCLUSIONS:
Despite concerns for impaired healing, NAC was not associated with increased high-grade wound complications and may even be protective after adjusting for comorbid factors. These findings support continued NAC use and further study of recovery optimization.
Back to 2025 Abstracts