Back to 2025 Abstracts
Contemporary Outcomes of Repeat Transurethral Resection among Patients with Non-Muscle Invasive Urothelial Carcinoma of the Bladder
Agustin Perez-Londono, MD1, Sumedh Kaul, MS
1, Aaron Fleishman, MPH
1, Ruslan Korets, MD
1, Heidi Rayala, MD, PhD
1, Peter Chang, MD, MPH
1, Andrew Wagner, MD
1, Joaquim Bellmunt, MD, PhD
2, Aria F. Olumi, MD
1, Boris Gershman, MD
1.
1Beth Israel Deaconess Medical Center, Boston, MA, USA,
2Dana-Farber Cancer Institute, Boston, MA, USA.
BACKGROUND: Repeat transurethral resection (re-TURBT) is recommended for intermediate- and high-risk bladder cancer to improve staging and oncologic outcomes. However, contemporary evidence on the role of re-TURBT is lacking. We therefore examined the contemporary rates of upstaging at re-TURBT and the association of re-TURBT with disease recurrence and progression among patients with high-risk bladder cancer.
METHODS: We identified patients with an incident diagnosis of high-grade Ta (HGTa), low-grade T1 (LGT1) and high-grade T1 (HGT1) urothelial carcinoma of the bladder between 2010 and 2022 at our institution. We examined pathologic findings at re-TURBT and evaluated the associations of re-TURBT with disease recurrence and progression using Cox regression.
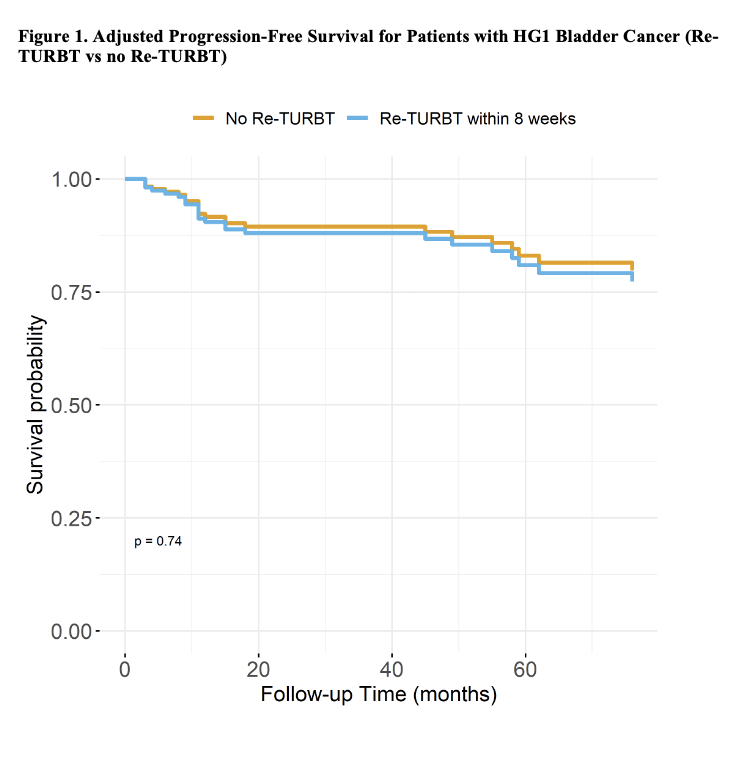
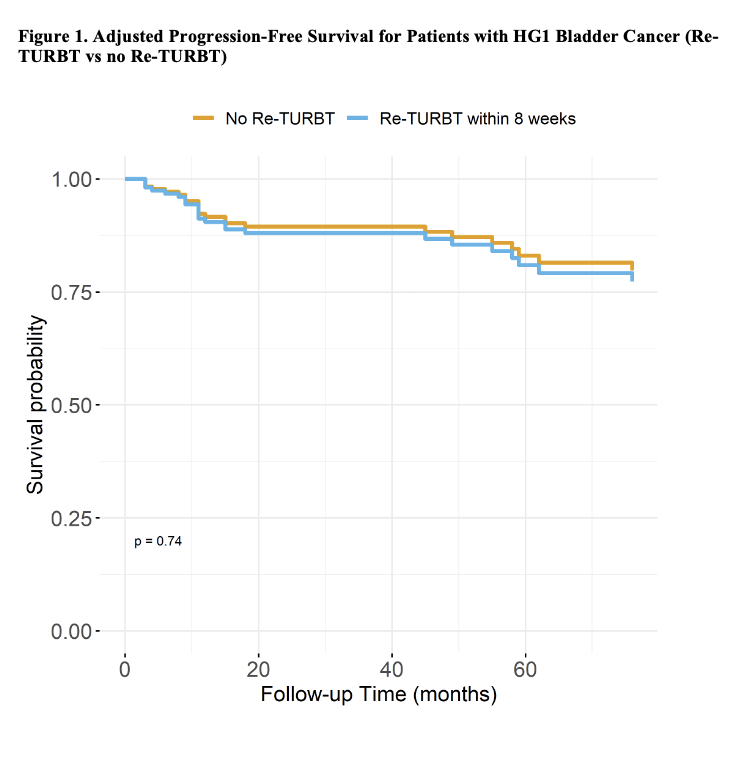
RESULTS: A total of 328 patients were included, of whom 88 (27%) underwent re-TURBT. At re-TURBT, 107 (33%) had HGTa, 209 (64%) had HGT1 and 12 (4%) had LGT1 disease. Among those who underwent re-TURBT, 9 (10%) patients were upstaged to ≥T2 disease, while 39 (44%) patients were found to have residual non-muscle invasive disease. Median follow-up time was 13 (IQR 6-39) and 24.5 (IQR 8-57) months for RFS and PFS respectively. In multivariable analysis, re-TURBT was not associated with a significant difference in disease recurrence (HR 1.0, 95% CI 0.58-1.71) or progression (HR 1.16, 95% CI 0.48-2.84) compared with no re-TURBT
(Figure 1).CONCLUSIONS: In a contemporary cohort of patients with bladder cancer, the rate of upstaging to ≥T2 at re-TURBT was 10%, lower than in historical studies, although the rate of residual non-muscle invasive disease remains high at 44%. Despite this, re-TURBT was not associated with a statistically significant difference in disease recurrence.
Back to 2025 Abstracts