Back to 2025 Abstracts
Does ureteroeneteric anastomosis stenting for radical cystectomy reduce ureteral stricture?
Muhieddine Labban, MD
1, Nathaniel F. Hansen, MD
1, Guilherme Garcia Barros, MD
2, Zhiyu (Jason) Qian, MD
1, Nnamdi Onochie, BS
1, Christopher Magnani, MD
1, Christopher P. Dall, MD
1, Jose Nolazco, MD
1, Mark A. Preston, MD, MPH
1, Matthew Mossanen, MD, MPH
1, Timothy N. Clinton, MD
1.
1Brigham and Women's Hospital, BOSTON, MA, USA, 2University of São Paulo, São Paulo, Brazil.
BACKGROUND: Recent data suggests that stenting across ureteroeneteric anastomosis during radical cystectomy (RC) with urinary diversion may not be necessary. Over time, we have gradually incorporated this approach into our practice. Herein, we examined whether the use of ureteral stenting reduces the risk of ureteral stricture.
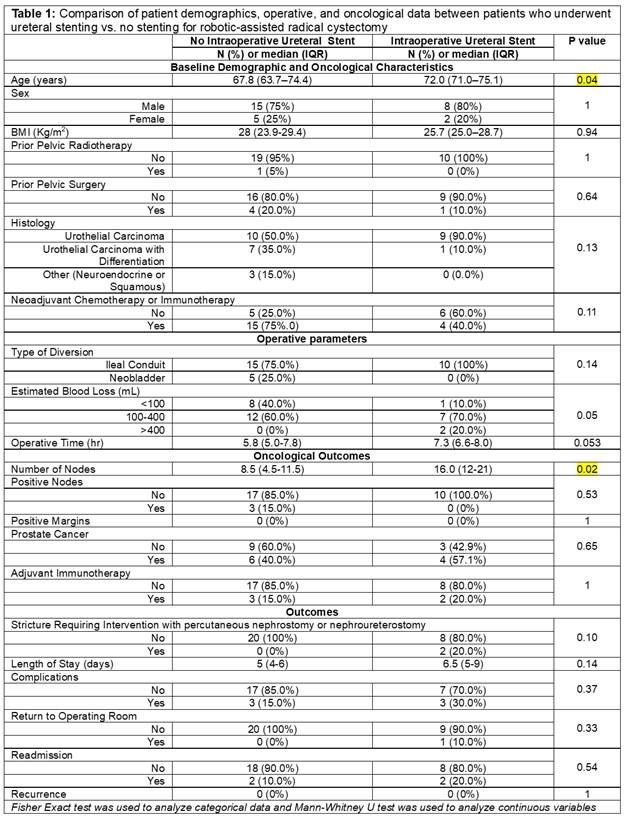
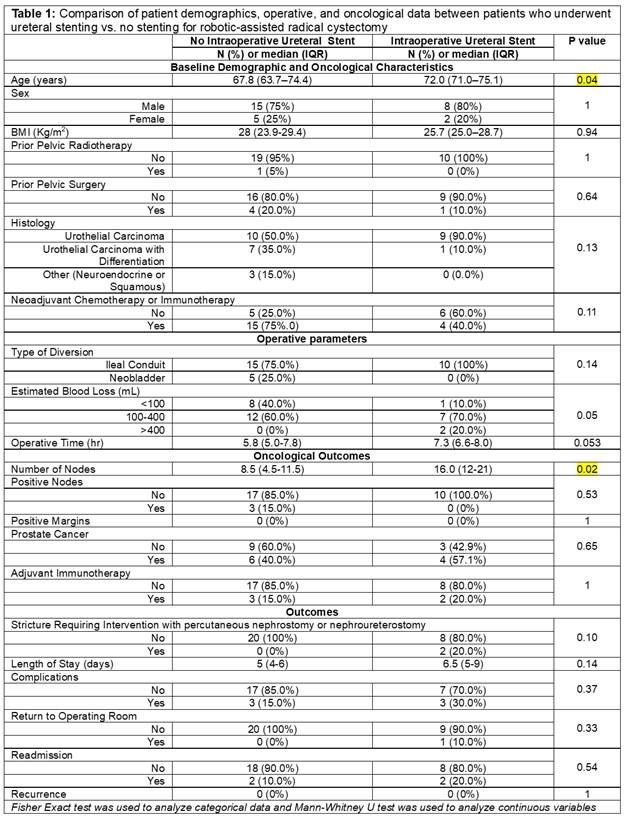
METHODS: A retrospective analysis of prospectively collected data was performed for patients who underwent robotic-assisted RC with urinary diversion performed by a single surgeon at a large academic center (9/2022-03/2025). We compared patient demographics and oncological characteristics between stent and no-stent groups. The primary outcome was ureteral stricture requiring intervention with percutaneous nephrostomy/nephroureterostomy. Secondary outcomes included length of stay, complications, readmission, return to OR, and oncological recurrence.
RESULTS: Among 30 patients, 10 (33.3%) had intraoperative ureteral stenting all of whom underwent RC with ileal conduit. The stent group was older (p=0.04), but there was no difference in other demographics including prior pelvic radiation (p=1) or pelvic surgery (p=0.64) (Table 1). There was no difference in operative time (p=0.08). The stent group had more lymph nodes dissected (p=0.02), but other pathological findings were similar (Table 1). Only 2/30 (6.7%) patients had stricture requiring intervention (44 and 714 days) both of which had received intraoperative stents (p=0.10). The rate of recurrence was nil across both groups but follow-up time was longer among the stent group [568 days (245-767) vs. 105 (25.5-155); p <0.001). Complications rates were similar across both groups (p=0.37) and only one patient had a hernia requiring reoperation (p=0.33).
CONCLUSIONS: Forgoing stenting for RC may be safe in the hands of an experienced surgeon. We aim to use these findings as proof of concept for a randomized clinical trial.
Back to 2025 Abstracts