Back to 2025 Abstracts
Association of Social and Emotional Support with Mental Health Outcomes Among Prostate Cancer Survivors: A Nationally Representative Analysis of 2023 BRFSS Data.
Jose I. Nolazco, MD, MMSc1, Juliana Villannueva-Congote, MD
1, Zhiyu (Jason) Qian, MD
1, Muhieddine Labban, MD
1, Christopher P. Dall, MD
1, Federico Lavagno, MD
2, Eugene Chen, BA
3, Guilherme Garcia Barros, MD
4, Matthew Mossanen, MD, MPH
1, Aaron H. Lay, MD
1, Timothy N. Clinton, MD
1, Adam S. Feldman, MD, MPH
1, Steven L. Chang, MD, MS
1.
1Mass General Brigham, Boston, MA, USA,
2University of Turin, Turin, Italy,
3Medical College of Wisconsin, Milwaukee, WI, USA,
4University of São Paulo, São Paulo, Brazil.
BACKGROUND: While survival rates for prostate cancer (PC) are high, many PC survivors experience considerable mental health challenges that negatively impact their quality of life. Evidence indicates that perceived social and emotional support (PSES) can enhance psychological resilience and overall well-being in cancer survivors; however, the specific effects of PSES on mental health outcomes among PC survivors are not well understood. This study aims to explore the association between PSES and mental health outcomes in this population.
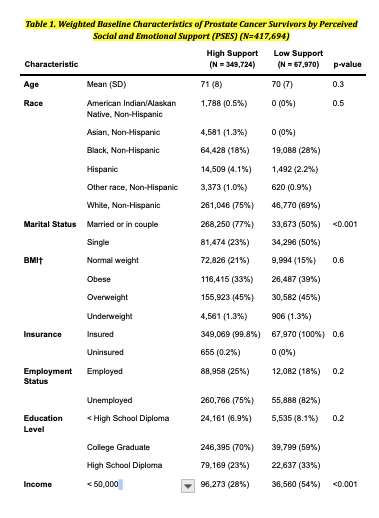
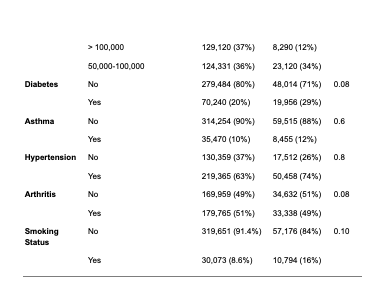
METHODS: We conducted a cross-sectional analysis using data from the 2023 Behavioral Risk Factor Surveillance System (BRFSS). The sample included 1,131 prostate cancer survivors. The primary exposure was perceived social and emotional support (PSES; high vs. low), and the primary outcome was self-reported mental health (poor vs. good). Survey weights were applied to obtain nationally representative estimates. Weighted multivariable logistic regression model was used to evaluate the association between PSES and mental health outcomes, adjusting for demographic, socioeconomic, and health-related covariates.
RESULTS: Among the weighted sample (N = 417,694), 16.3% reported low PSES, and 25.5% reported poor mental health. In the weighted adjusted model, low PSES was independently associated with poor mental health (adjusted OR: 1.96; 95% CI: 1.05-3.63; p = 0.034) after accounting for age, race, marital status, BMI, income, education, comorbidities, and smoking.
CONCLUSIONS: In this nationally representative sample of prostate cancer survivors, we found a significant association between low PSES and poor mental health in PC survivors, highlighting the need to incorporate assessments of social and emotional support to PC survivors.
Back to 2025 Abstracts