Back to 2025 Abstracts
Center-based endophycity measurement improves interobserver agreement of the RENAL nephrometry score
Clara E. Goebel, MS31, Keenan Moore, MS4
2, Nicholas Heller, PhD
3, Jayant Siva, BS/MD Student
3, Jamee Schoephoerster, MD
4, Griffin Struyk, MD
5, Nitin Venkatesh, MD
6, Beatriz Lopez Morato, Medicral Student
7, Christopher Weight, MD
3.
1University of Vermont Larner College of Medicine, Burlington, VT, USA,
2Loyola University Chicago, Maywood, IL, USA,
3Cleveland Clinic, Cleveland, OH, USA,
4Oregon Health & Science University, Portland, OR, USA,
5HealthPartners Regions Hospital, St Paul, MN, USA,
6Oakland University, Auburn Hills, MI, USA,
7Autonomous University of Madrid, Madrid, Spain.
BACKGROUND: Since its introduction, the RENAL nephrometry score has proven to be an effective tool in medical decision making and surgical planning for renal tumors, shown to be predictive of several oncologic and operative outcomes. However, studies have shown high interobserver variability within RENAL’s endophycity (“E”) portion. Here, we propose the use of center-based endophycity (CBE) in place of RENAL “E” to improve interobserver agreement while maintaining utility.
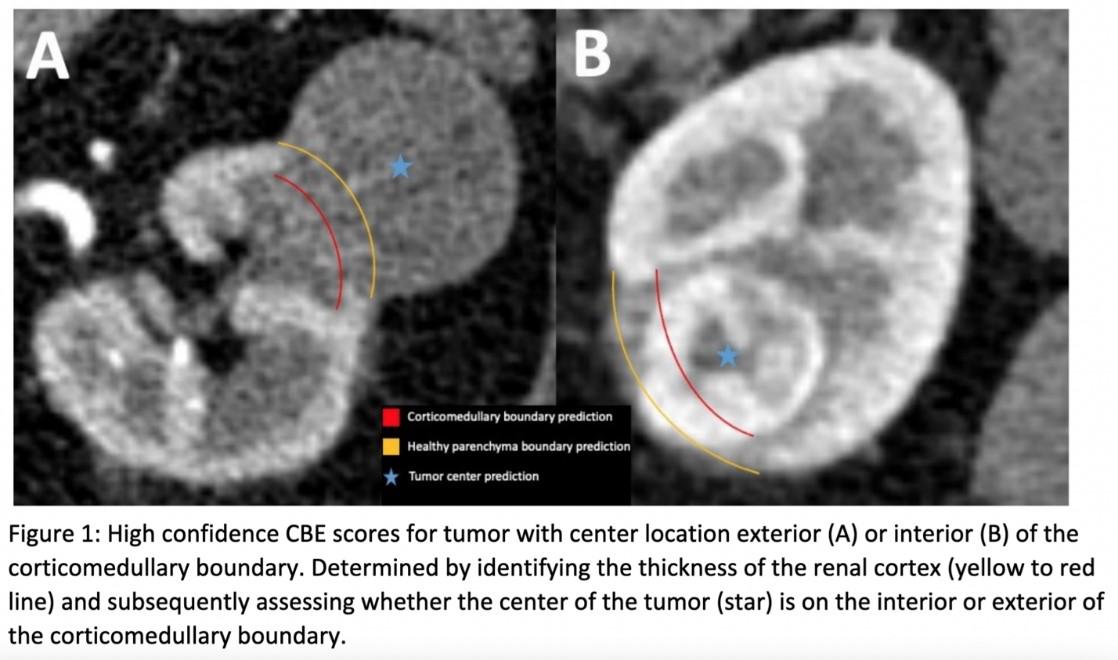
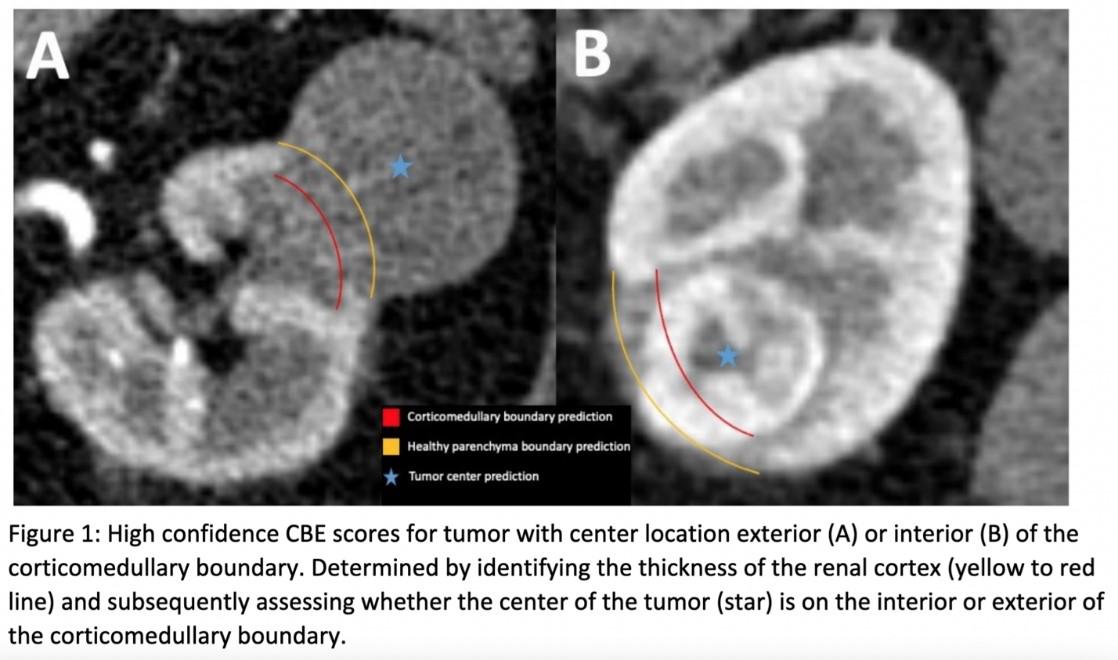
METHODS: Medical records for patients who underwent radical or partial nephrectomy for suspected renal malignancy at a single institution over 9 years were retrospectively collected. Six independent observers manually assigned each case RENAL scores and three observers assigned CBE scores. CBE was determined by approximating the endophycity of the tumor’s center by its location relative to the corticomedullary boundary. Exophytic and endophytic tumors were scored “1” and “2”, respectively. Interobserver agreement was analyzed using the kappa coefficient, and logistic regression was used to predict outcomes.
RESULTS: 288 cases met inclusion criteria. CBE scoring (kappa coefficient 0.77) showed significantly higher interobserver agreement than RENAL “E” (kappa coefficient 0.17, p < 0.0001). Both RENAL and RENAL with CBE predicted ISUP grade (p<0.0001, p<0.0001), tumor necrosis (p<0.0001, p<0.0001), and perioperative blood loss (p=0.001, p<0.0001). RENAL predicted malignancy (p=0.001), while RENAL with CBE did not (p=0.058). However, CBE independently predicted malignancy (p=0.039) unlike RENAL “E” (p=0.365).
CONCLUSIONS: These results suggest that RENAL “E” is susceptible to particularly low interobserver agreement. CBE scoring provides a more reproducible alternative to RENAL “E” while preserving many of RENAL’s predictive capabilities. Further studies are needed to elucidate these thus far insignificant yet promising findings and confirm them in additional studies.
Back to 2025 Abstracts