Back to 2025 Abstracts
Urology Workforce Shortages: Increasing Transfer Burden on Tertiary Care Centers
Orleiquis Guerra, MD, Elisa Rocha, MD, Jennifer Fantasia, MD, Jennifer K. Yates, MD, Mitchell Sokoloff, MD.
University of Massachusetts, Worcester, MA, USA.
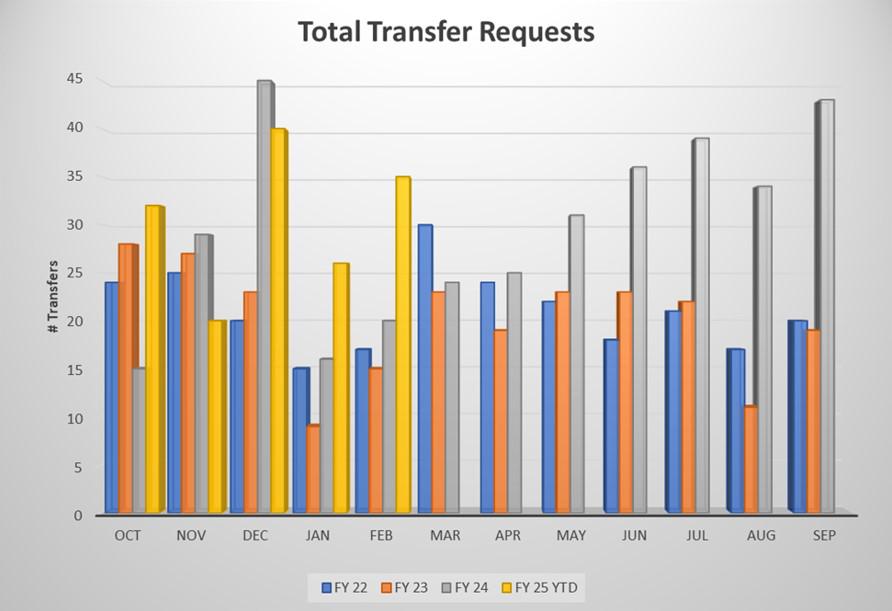
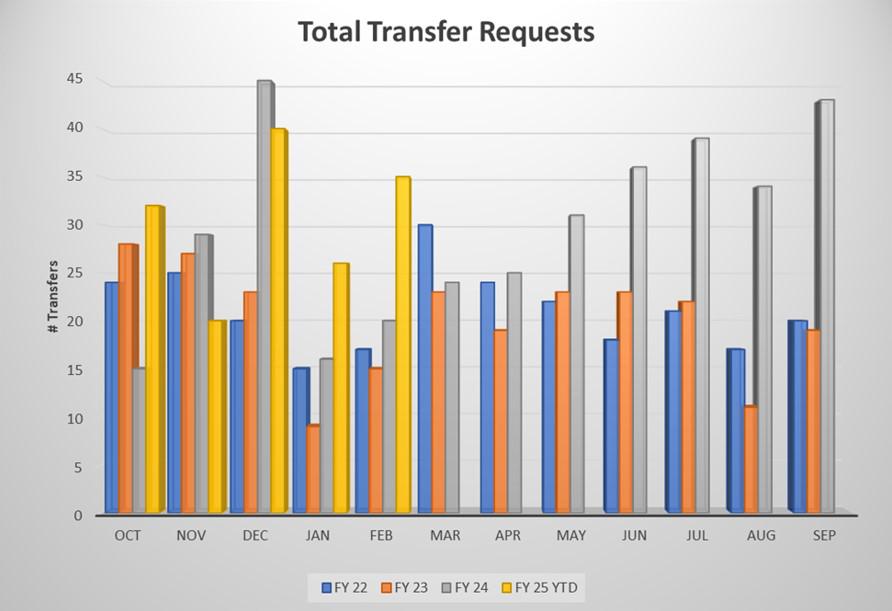
Introduction: Urology is a specialty facing a critical ongoing physician shortage. This shortage has led to increasing patient transfers to tertiary care centers, delaying treatment, taxing on-call providers and compounding financial strain. We present how the Urology workforce shortage in Central Massachusetts has impacted transfer volumes and associated cost to our tertiary referral center, UMass Memorial Medical Center (UMMMC). Methods: We analyzed urology-related transfer requests recorded by the transfer center at UMMMC from Fiscal Year (FY) 2022 through the first five months of FY 2025. The catchment area includes 6 community hospitals generating the majority of transfers/transfer requests, and several additional community hospitals contributing a smaller number of requests. Two of these hospitals have no urology coverage, the other four hospitals have minimal coverage. Total cost of transfers between hospitals was estimated using an approximated transportation fee of $2,500 per transfer. Results: A total of 1,128 urology transfer requests were recorded over 41 months. Transfer requests increased by 53% from FY 2022-2023 to FY 2024. In the first five months of FY 2025, 166 transfers had already been logged, indicating a continued upward trend. This corresponds with decreased call coverage in the community. The direct transportation cost over the 41 months period was calculated at $2.8 million. Conclusion: The declining availability of urology coverage in Central Massachusetts has led to increased transfers to the regionís only tertiary care, delaying care and straining resources. This trend aligns with the known increase in retirement of community urologists and is likely occurring nationally. Urgent policy solutions are needed to address workforce shortages, improve regional coverage, and reduce financial and logistical pressures on healthcare systems.
Back to 2025 Abstracts