Back to 2025 Abstracts
The Price of Coverage: Insurance Disparities in Testicular Torsion Outcomes Across Ten Years of Statewide Data
Loren J. Smith, M.D.1, Jacqueline Klepinger, B.S.
2, Evelyn James, B.S., M.P.H.
1, Lily C. Wang, M.D., Ph.D.
1.
1MaineHealth Maine Medical Center, Urology, Portland, ME, USA,
2University of New England, College of Osteopathic Medicine, Biddeford, ME, USA.
Background Acute testicular torsion (AT) is a urologic emergency requiring prompt surgical intervention to maximize testicular salvage. While hospital characteristics and time to surgery are known factors, the influence of socioeconomic disparities remains understudied. This study examines the impact of hospital size, time to surgery, distance to care, and insurance type on orchiectomy rates in AT.
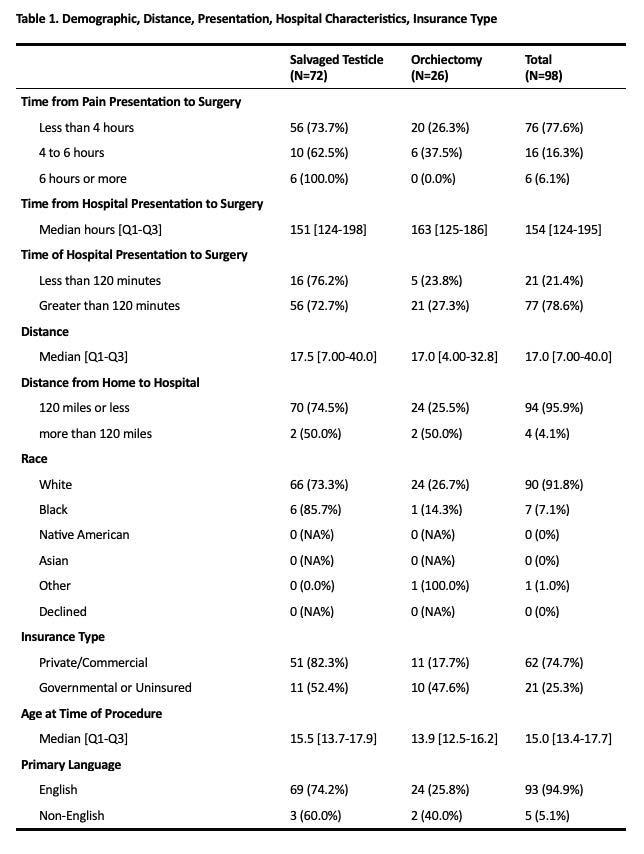
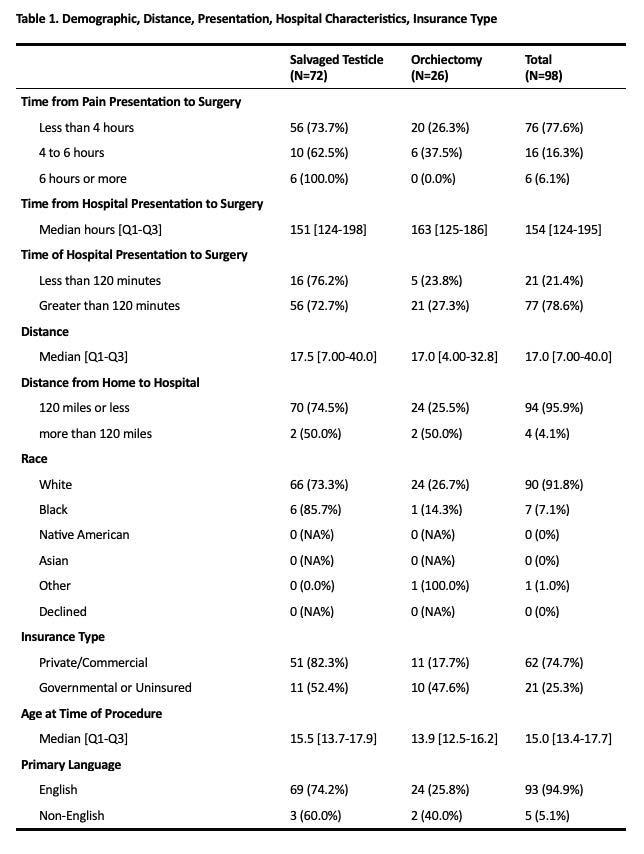
Methods A retrospective review of patients diagnosed with AT between 2013 and 2023 within a statewide hospital system was conducted. Demographic and perioperative data were collected. Logistic regression was used to identify predictors of orchiectomy.
Results Among 98 patients (median age 15 years), 74.7% had private/commercial insurance, and 25.3% had government insurance or were uninsured. Median time from hospital presentation to surgery was 154 minutes. On regression analysis, hospital size (OR 1.50, p=0.5), distance from home to hospital (OR 2.41, p=0.4), and time from presentation to surgery (OR: 1.35, p=0.6), were not significant predictors of orchiectomy. However, patients with government or no insurance had significantly higher odds of orchiectomy compared to those with private or commercial insurance (OR 4.21, 95% CI 1.44-12.6, p=0.009).
Conclusions Patients with private and commercial insurance had significantly higher rates of testicular salvage in AT. Insurance status was the only statistically significant predictor of testicular loss in our analysis. In the U.S., insurance type often reflects broader socioeconomic conditions, which prior research has linked to differences in education and health literacy. Although time to surgery and distance to care were not statistically significant in this cohort, they remain clinically relevant. Our findings suggest that socioeconomic factors may be critical in preventing testicular loss.
Back to 2025 Abstracts